Introduction
The prevalence of type 2 diabetes showed a significant growth, from 7% to 9.2%, between 2006 and 2012 (National Health and Nutrition Survey [ENSANUT], 2012). Such an increment has been apparent in the higher demand for hospital and ambulatory services, a higher rate of patients with acute and chronic complications, an increase in the mortality derived from complications, and in the increasing expenses on medical attention. Prevention, providing high quality treatment and metabolic control of diabetes patients are the priorities of the Mexican health sector (Córdova-Villalobos et al., 2008; Secretaría de Salud, 2006).
Patient’s self-care through the adherence to drug and non-drug treatments, such as regular physical exercise and a healthy way of eating, allows to achieve control of diabetes, delay its complications, reduce disabilities and increase life expectancy (World Health Organization [WHO], 2014). Unfortunately, the proportion of patients with optimal self-care practices is very low. In Mexican patients, adherence to drug treatment is 78.4%; to regular physical exercise, 44.3%; and to eating low contents of sugar and high contents of vegetables, 58% (Lerman et al., 2004). Such figures partly account for the fact that only 29.7% of the patients reach glycemic control (Flores-Hernández et al., 2015).
In the individual realm, there are three groups of factors associated with the low adherence to self-care. The first group includes those factors related to the disease and its treatment, such as the duration of the illness, presence of comorbidity, acute and chronical complications, number and frequency of medication use. The second group involves intrapersonal factors such as gender, age, self-efficacy, psychological (e.g. distress), and psychiatric factors (e.g. depression). The third group comprises interpersonal factors such as physician-patient communication and the social support the patient has (World Health Organization [WHO], 2014).
Diabetes provokes relevant psychological responses in patients. People with diabetes frequently feel frustrated, angry, discouraged, stressed, and anxious, and may develop some emotional disorder due to various reasons such as the diagnosis of the disease, the emergence of complications, difficulties for carrying out a treatment regime as well as other stressful events in their surroundings (Polonsky et al., 2005). Responses to environmental stressors and to those related to the disease may range from some positive adaptation called eustress to a negative response called distress, which overcomes the abilities of the patients and the situation they have to face (Selye, 1974). Thence, distress in diabetic patients is defined as an emotional upsetting load (non-psychiatric) secondary to the disease, which has not yet gone further into a more severe clinical profile (Fisher, Hessler, Polonsky & Mullan, 2012).
Studies carried out in the United States (Gonzalez, Shreck, Psaros & Safren, 2015; Hessler et al., 2014; Franks et al., 2012) and Nigeria (Ogbera & Adeyemi-Doro, 2011) have found that people suffering diabetes and distress have a greater risk of presenting low adherence to self-care in comparison with patients who do not.
In Mexico, research in diabetic patients has focused on psychiatric disorders such as anxiety and depression (Lerman et al., 2004; Fabián, García & Cobo, 2010; Serrano, Zamora, Navarro & Villarreal, 2012; Castro, Tovar & Mendoza, 2009; Sánchez, Hipólito, Mugártegui & Yáñez, 2016; León, Guillen & Vergara, 2012). Distress has received little attention in this population (Lerman et al., 2009). However, considering its relation to diabetes, it is convenient to analyze its magnitude, that is, the frequency of distress and its relation to the lack of adherence to treatment in Mexican patients. Therefore, the purpose of the present study was the assessment of the frequency of distress and its association with deficient self-care in Mexican patients with type 2 diabetes.
Method
A study was carried out; its design was cross-sectional (measurement of all variables), bilective (gathering of data in files and interviews to diabetic persons), retrospective (the subjects assessed were asked to locate themselves temporarily in a unit of a month prior to evaluation); homodemic (population beneficiary of the Mexican Institute of Social Security [IMSS]); multicentric (sample was obtained in two family practice clinical centers); and analytical (for its scope in the analysis and explanation of the relation between variables). The study was carried out between January and June 2014. The two family practice clinics were selected based on convenience, one in the North and the other in the South part of the city. Both family practice clinics have 30 offices and the same services and infrastructure (outpatient area, preventive medicine, emergency area, clinical laboratory, drugstore). These clinics cover approximately 1.4 million people.
Participants
The sample included 489 people with type 2 diabetes. Inclusion criteria were being older than 19 years of age, having at least a three-month diagnosis and accepting to participate in the study by means of a letter of informed consent.
People with cognitive alterations were not included in the study; this was confirmed by asking patients whether they had any memory issues as well as by reviewing files in relation to medical diagnosis of dementia or mental retardation. Finally, no patients were included with a diagnosis of schizophrenia, psychosis, disorders related to the use of substances (substance induced delirium, amnesic disorder, substance induced mood disorder), or bipolar disorder.
Two nurses received one week of training to perform field work. Training included strategies for the identification and recruitment of participants and questionnaire administration. Nurses were in charge of identifying patients with diabetes who fulfilled inclusion criteria, inviting them to take part in the study, administering the questionnaire and verifying diagnosis and treatment in the participants’ files. Nurses also interviewed type 2 diabetes patients who attended the clinic during the morning and afternoon shifts at the time of the study and who accepted answering the questionnaire.
The project was approved by the National Committee for Research and Ethics of the IMSS (number R2013-785-034).
Measurement instruments and study variables
Distress secondary to diabetes was the independent variable. Distress was defined with the Distress Scale for patients with Diabetes and Hypertension (DSDH17M) (Martínez, Doubova, Aguirre & Infante, 2016) which is an adaptation of the Diabetes Distress Scale (DDS17) designed in the United States (Polonsky et al., 2005). Both the DDS and the DSDH17M include 17 items under three domains (distress related to the treatment regime, interpersonal distress and distress related to the physician). Each item is graded with a six-point scale ranging from “it is not a problem” to “a very serious problem”. Total score is the sum of the items divided by the total number of items. According to Fisher et al. a score ≥ 3 points out to the presence of emotional distress (Fisher et al., 2012).
A deficient self-care of the patients was conceptualized by means of three dependent variables: 1. Low adherence to drug treatment, when the patients reported not complying with the dosage or hours indicated for drugs prescribed the previous month; 2. lack of regular physical exercise, when the patients answered they did not engage in or engaged in less than three thirty-minute sessions per week (so that this variable was operating when we used the criteria of the guide for the prescription of physical exercise for patients with cardiovascular risk, which takes into account patients with diabetes) (Abellán, Sainz de Baranda & Ortín, 2014); 3. lack of a proper diet, which was identified by means of two variables defined from recommendations of the Clinical Practice Guideline, Diagnosis and treatment of type 2 diabetes mellitus (2012). Variables were: a) low intake of vegetables, defined as an intake lower than four rations of vegetables per day, and b) frequent intake of food and beverages with high sugar content. A frequent intake was defined when the participant reported consumption of food and beverages with high sugar content, three or more times per week.
Relevant co-variables related to self-care were grouped into five categories: 1. Sociodemographic characteristics, 2. health condition, 3. behavior related to health, 4. general self-efficacy, and 5. information about self-care.
1. Sociodemographic characteristics included: gender, age group (0 = < 65 and 1 = ≥ 65 years), schooling (1 = primary school or less, and 0 = secondary or higher), job (1 = paid job or 0 = no paid job or retired).
2. Health condition included: duration of diabetes ≤ 3 years after diagnosis, presence of comorbidity such as hypertension, presence of any diabetes complication; probable depression and/or anxiety, and number of drugs prescribed: < 3 (codified as 0) or ≥ 3 (codified as 1). Depression and anxiety were assessed with the Hospital Anxiety and Depression Scale (HADS). This scale is a screening instrument which assesses depression and anxiety in non-psychiatric hospital environments. HADS has 2 subscales (depression-7 items and anxiety-7 items) and its items have Likert 4 point answers. Sum score per subscale is 0 to 21 points. Scores ≥ 11 identified probable anxiety or depression (Nogueda, Pérez, Barrientos, Robles & Sierra, 2013).
The presence of contraindications to engage in physical exercise was identified as specified in the guidelines for prescription of physical exercise for patients with cardiovascular risk (Abellán et al., 2014). Contraindications included cardiovascular ailments such as recent myocardial infarction, or any other acute cardiac event, unstable angina, uncontrolled cardiac arrhythmia, severe symptomatic aortic stenosis, uncontrolled symptomatic cardiac insufficiency, acute pulmonary embolism or lung infarction, acute myocarditis or pericarditis, aneurysm, moderate stenosis, electrolyte abnormalities (hypokalemia, hypomagnesemia), severe arterial hypertension (systolic arterial pressure > 200 mm Hg or diastolic arterial pressure > 110 mm Hg at rest), hypertrophic cardiomyopathy, and rheumatoid disorders exacerbated by exercise, auriculoventricular block, or aneurysm, apart from physical or mental handicap generating inability to perform exercise adequately.
3. Behavior related to health focused on smoking and alcohol intake. Tobacco addiction was classified as 1 = smoker of at least one cigarette per day, and 0 = nonsmokers. Alcohol consumption was classified as nondrinkers (never drank alcohol), occasional drinkers (who hardly ever drank or less than once a week), moderate drinkers (1 to 14 drinks per week) and intense drinkers (over 14 drinks per week) (Clemens, Matthews, Young & Powers, 2007). Due to the low proportion of moderate and intense drinkers (n = 28), they were grouped with the occasional drinkers and data was presented as 0 = does not drink alcohol, and 1 = drinks alcohol.
4. The self efficacy of the patient was assessed with the General Self-efficacy Scale. This scale has 10 4-point Likert answer items and has been translated and validated in 28 different languages, including Spanish. This scale measures a person’s perception regarding his/her ability to handle with efficacy different stressing situations. A ≤ 19-point score means lack of self efficacy (Schwarzer & Jerusalem, 1995; Cid, Orellana & Barriga, 2010).
5. Information regarding self-care was determined by identifying whether the patient had received and understood information about: a) dosage and/or hours for drug treatment; b) adverse reactions to medication; c) reasons to engage in physical activity; d) kinds of physical activity, time per session and frequency per week; e) importance of the increase in daily intake of vegetables; f) reasons for increasing intake of vegetables; g) importance of diminishing intake of foods with high sugar content. These variables were codified as 1 if the patient had not received or understood the information and 0 if the patient had received and understood the information.
Sample size
Sample size was based on the practice which ascertains 30 participants for every variable included in the multiple regression model (Wilson & Morgan, 2007).
Statistical analysis
Descriptive statistics was used to characterize the population of the study. Later on, a bivariate analysis with square chi test was applied to compare frequency between the independent variable (distress) and the co-variables among groups of patients according to dependent variables (for example, distress frequency in patients with or without low adherence to drug treatment; in patients with or without lack of regular physical exercise, etc.) Finally, to estimate the independent association between distress and each one of the dependent variables, we built multiple Poisson regression models with a heavy variance estimator for each dependent variable. This statistical model offers direct calculations of the reasons of prevalence and their 95% confidence intervals, as the best alternative for logistic regression in cross-sectional studies with binary results, when the result of interest is common (> 10%) (Barros & Hirakata, 2003). Construction of multivariate models considered conceptually that the independent variable and the co-variables are clinically relevant in accordance to literature related to this topic.
Results
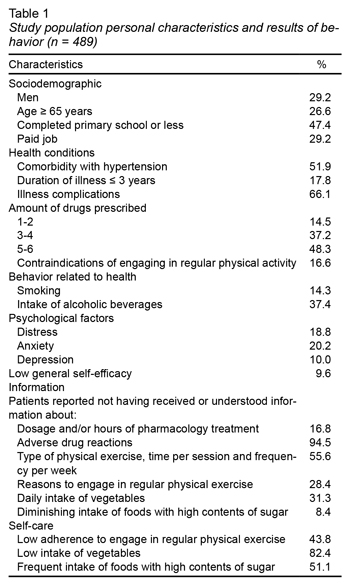
Table 1 describes the characteristics of the 489 diabetic patients who participated in the study. Less than one third were men, 65 years or older, with low schooling and a paid job. Only 17.8% had a recent diagnosis of diabetes. Over half of them had comorbidity with hypertension and diabetes complications. Distress was identified in 18.8%; also, 20.2% scored for possible anxiety and 10.0% for depression (such percentages were obtained with a screening instrument and not by means of psychiatric assessment). Low adherence to drug treatment was identified in 44.8%, while 43.8% did not engage in regular physical exercise. From the total, 82.4% had low vegetables intake and 51.1% frequently consumed food with a high sugar content. However, only 9.6% had lack of general self-efficacy.
As for information regarding self-care, 16.8% of the patients had not received or understood the information about the drug treatment regime, 94.5% about possible adverse effects of the medication, 28.4% about the reasons to engage in regular physical exercise, 55.6% about the kind of exercise and the length and frequency of the weekly sessions, 31.3% about the importance of increasing their daily intake of vegetables and 8.4% about the relevance of diminishing the consumption of foods with a high sugar content.
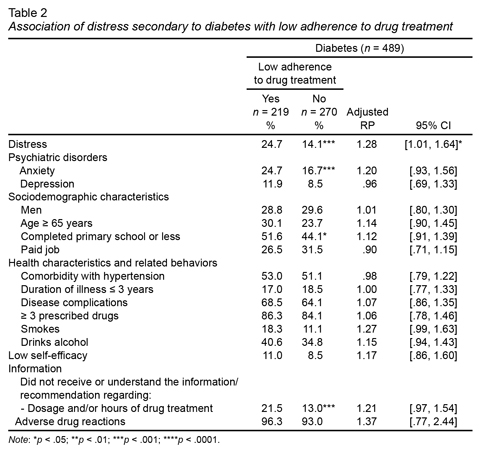
Table 2 presents the results of the bivariate and multivariate analysis of the association of distress and other conceptually relevant covariables with the low adherence to drug treatment. Bivariate analysis showed that the group of patients with low adherence to treatment were those who had distress and anxiety, who had not finished their primary school and who had not understood or received the information about doses and hours of the drug treatment.
Multivariate analysis showed that patients with distress had greater probability (24.7%) of presenting low adherence to drug treatment (95% CI [1.01, 1.64]).
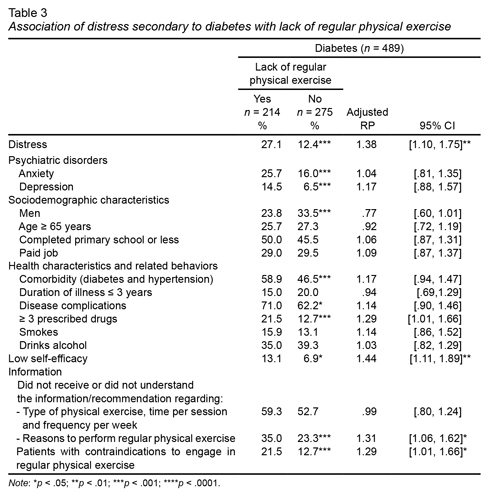
Table 3 shows that patients with distress had a 27% greater chance of not engaging in regular physical exercise (95% CI [1.01, 1.75]). Other associated factors were: lack of self-efficacy (RP 1.44; 95% CI [1.11, 1.89]), not having received or understood the reasons to engage in physical activity (RP 1.31; 95% CI [1.06, 1.62]) and having contraindications for engaging in regular aerobic physical exercise (RP 1.29; 95% CI [1.01, 1.66]).
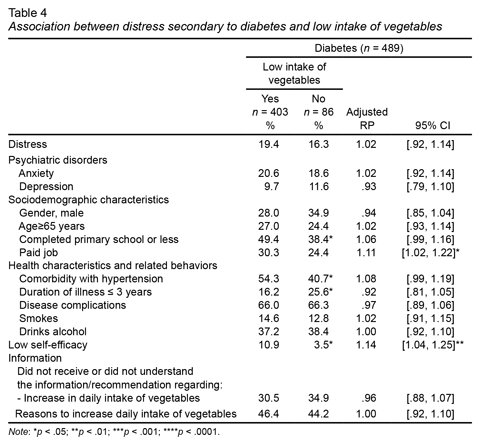
Table 4 shows there was no association between distress and low intake of vegetables. Factors associated with low intake of vegetables were: paid job (RP 1,08; 95% CI [1.02, 1.22]) and lack of self-efficacy (RP 1.14; 95% CI [1.04, 1.25]).
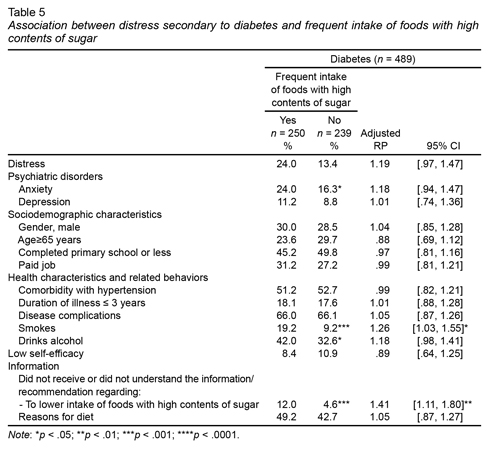
Table 5 shows there was no association between distress and frequent intake of foods with high contents of sugar. Variables associated to this variable were: smoking (RP 1.26, 95% CI [1.03, 1.55]) and not having received or understood the recommendation of diminishing consumption of food with a high sugar content (RP 1.41, 95% CI [1.11, 1.80]).
Discussion and conclusion
The present research shows that two out of every 10 patients with type 2 diabetes suffered from distress, which was associated with low adherence to drug treatment and lack of regular physical exercise.
We found that the emotional load secondary to diabetes is shown on a greater prevalence of distress (18.8%) and possible psychiatric disorders, such as anxiety (20.2%) and depression (10%). Such numbers are greater if compared to general population, where prevalence of anxiety is 14.3%, distress ranges between 3.4% and 12%, and depression is 7.8% (Medina-Mora et al., 2003; Weissman, Pratt, Miller & Parker, 2015; Moriarty, Zack, Holt, Chapman & Safran, 2009; Doherty, Moran & Doherty, 2008). Data on prevalence of anxiety and depression came from Mexico; however, the referent for prevalence of distress came mainly from the United States, since these data are not available for Mexican population. At the same time, prevalence of affective disorders (anxiety and depression) found in the present study is similar to the figures reported in similar studies (Fisher et al. 2012; Sturt, Dennick, Due-Christensen & McCarthy, 2015; Fisher, Glasgow & Strycker, 2010).
In our study, distress in diabetic patients was associated with poor adherence to medication and lack of regular physical exercise. Such results are in accordance with several studies from the United States, which found an association of distress with low adherence to medication (Aikens, 2012), and the lack of regular physical exercise (Shin, Chiu, Choi, Cho & Bang, 2012).
Some researchers have pointed out that possible paths for the relation between stress and adherence to self-care might be a low motivation in chronic patients due to an erroneous perception of the low risk of not adhering to treatment, as well as the patient’s feeling of inability to have an impact on the disease, which is perceived in low self-efficacy (González et al., 2015; Berry, Lockhart, Davies, Lindsay & Dempster, 2015). Thence, detection and psychological support for handling distress in diabetic patients may be an essential step for promoting self-care (González et al., 2015; Castro et al., 2009; Laaksonen et al., 2005).
Consistently with other studies, we did not find an association between distress and intake of vegetables and sugar. For instance, one study in the United States reported that depression and not distress was significantly associated with intake of a healthy diet in type 2 diabetes patients (Berry et al., 2015). In the case of our study, no psychological factors, including depression and anxiety, were linked to the intake of vegetables and sugar. Deficiencies in this component of self-care were associated to low self-efficacy and lack of information.
Offering information and education to patients about self-care is essential to improve their health condition. We found that a high percentage (between 16.8% and 94.5%) of the patients in our study informed not having received or understood the information regarding some of the points of their self-care. Besides, failures in the provision of information were associated to low adherence to drug treatment, lack of regular physical exercise, and consumption of foods with high sugar content. These findings are coherent with previous studies which mentioned that not having received or understood the information about portions and the frequency of meals may be associated with low adherence to diet in diabetic patients (Ranasinghe et al., 2015; Cheng et al., 2016; Parajuli, Saleh, Thapa & Ali, 2014). Thence, it is important that the information provided to the diabetic patient has clear recommendations for self-care, expressed in a kind of language that the patient may fully understand. Myths or erroneous beliefs regarding self-care may increase due to lack of information, provoking the sensation of being deprived and denied medical recommendations (Cheng et al., 2016).
The high prevalence of distress in type 2 diabetes patients compared to general population and its association with self-care suggests the importance of its screening and care in family practice. Screening may be performed by trained health professionals (v.gr. nurses, social workers), followed by the attention of the problem identified by a psychologist. It is also relevant to test our findings with studies in other locations and populations in Mexico.
Also, the association between distress and low adherence to drug treatment and lack of regular physical exercise suggests that further multidisciplinary research be made, including specialists in different areas, with the purpose of carrying out in depth research of each one of the elements of distress and self-care.
Limitations
Among the limitations of this study, it is important to mention that, by being a cross-sectional study, it is impossible to establish a causality. However, the results of the study identify the magnitude of the issues of distress in diabetic patients, which allow for the planning of strategies to improve the well-being of this population. Another limitation of the study is that the aspects of self-care were assessed by means of self-reports and not through objective measuring (v.gr. counting the pills, measuring the concentration of prescribed medication in blood, measuring glycosylated haemoglobin), which may present a chance of memory bias and social desirability. The strategies to reduce such biases included: 1. having a non-inclusion criteria to patients with cognitive problems; 2. focusing the items of the questionnaire on self-care activities during the last month, and 3. confirming information by means of reviewing the clinical files. Thanks to these strategies, percentages of patients with low adherence to drug treatment, lack of regular physical exercise, and deficiencies in diet were similar to those found previously on diabetic patients in Mexico (Lerman et al., 2004; Krass, Schieback & Dhippayom, 2015; Faria et al., 2014; Mumu, Saleh, Ara, Afnan & Ali, 2014). On the other hand, the study sample was limited to patients in two family practice medical units of the IMSS, which prevents the study from being representative. However, due to the uniformity of the affiliation criteria to the IMSS and for the care of diabetic patients, which are based on institutional clinical guidelines, it is expected that the results may be generalized to the population of the IMSS, which is one of the largest health providers in Mexico.