Background
Gambling disorder (GD) is a relatively common and often disabling psychiatric condition characterized by intrusive urges to engage in deleterious gambling behavior in terms of time invested and money wagered, which results in significantly negative effects on gamblers daily lives and quality of life. DSM-5 criteria for gambling disorder focus on preoccupation with gambling, need to gamble increasing amounts of money, and repeated unsuccessful efforts to control gambling. Furthermore, relapse following the treatment is a common outcome (González-Ortega, Echeburúa, Corral, Polo-López, & Alberich, 2013; Kassani, Niazi, Hassanzadeh, & Menati, 2015).
The occurrence of GD varies from country to country and the measures for calculating the prevalence are not always the same. In general, about .8% - 1.5% of the adult population can be classified as probable individuals with GD while the prevalence of problem gambling is 2.5% (Kessler et al., 2008). Substance abusers and patients seeking treatment for psychological problems (e. g., anxiety and mood disorders) tend to have high rates of gambling problems (20%). In turn, individuals with GD often suffer from comorbid disorders, such as personality disorders (47.9%), mood disorders (23.1%), alcohol use disorders (21.2%), or anxiety disorders (17.6%) (Dowling et al., 2015).
Patients with dual disorders are highly prone to adverse outcomes in several domains (about 60%): increased rates of hospitalization, nonadherence to treatment and poor overall response to pharmacologic treatment (Green, Drake, Brunette, & Noordsy, 2007). Comorbid mental disorders are often undetected in individuals with GD, which can complicate their treatment (Ziedonis, Steinberg, Smelson, & Wyatt, 2009). The presence of GD and another mental disorder poses special diagnostic and treatment challenges. Thus, the personal, family and social problems of these patients increase and reduce gains of the treatment; patients may relapse or give up the therapy. Therefore, there is a need for comprehensive assessment and integrated intervention that addresses the multiple problems associated with these co-occurring disorders.
There are several reviews about the psychological treatment of GD in the literature, but there is only one mini-review about GD with different kinds of psychiatric comorbidities and with the main focus on drug treatment (Dowling, Merkouris, & Lorains, 2016). Therefore, the main aim of this research is to review existing evidence on the role of evidence-based psychological interventions for disordered gamblers with different co-occurring psychiatric disorders.
Method
A systematic search of original articles (2010-October 2017) was conducted in MEDLINE and PsycInfo. Key terms in title, abstract and keywords were: 1. gambling or gamblers, 2. treatment, intervention, therapy, or therapeutics, and 3. dual diagnosis or comorbidity. Four hundred and eight references were found. Regarding exclusion and inclusion criteria for the searched records, case studies, dissertations, letters to the editor, and duplicate records were removed from the analysis. Finally, empirical articles and other relevant documents in this topic dealing with adult patients were taken into account (meta-analysis research or reviews). The analytic plan is based on the search of relevant publications for this topic, the selection, reading, synthesis, and exposition of the state of the art.
Results
Psychological intervention for gambling disorder
Treatments for GD reported in the literature are quite similar to methods to treat other addictions. However, few empirically supported treatments for GD have been developed. Regarding treatment goals, complete abstinence versus moderated gambling is an issue that needs to be addressed. Both goals are necessary for different kinds of patients (Echeburúa & Fernández-Montalvo, 2005). While abstinent focused treatment programs are the best option for strictly individuals with GD, moderated gambling in a harm reduction approach may be interesting for problem gamblers.
Current treatment for GD involves a number of different options, including inpatient treatments, intensive outpatient, individual and group cognitive-behavioral options (CBT), and pharmacotherapy. Inpatient care is generally limited to patients with severe acute crises, treatment failures, and severe comorbid disorders, particularly depression and attempted suicide (Echeburúa, 2015).
Behavioral and cognitive-behavioral approaches
Behavioral approach takes into account three components of gambling behavior: antecedents (financial pressure, gambling cues, positive or negative emotions, interpersonal factors, urges to gamble), overt or covert behavior itself (coping strategies to deal with negative feelings, thinking about gambling), and consequences (autonomic arousal, opportunities to socialize, escape from personal problems, monetary gain to cope with financial loss) (Hodgins & Holub, 2007).
Behavioral therapy considers disordered gambling a learned behavior and relies on techniques such as stimulus control, systematic exposure, and skills development to reverse the learned behavior and the association between arousal and conditioned elicitors. Reduction in gambling is expected if patients can successfully develop and use alternative coping responses to deal with urges to gamble (Echeburúa, 2015).
Stimulus control involves limiting access to money, not visiting venues that offer gambling, and not spending time with people associated with heavy gambling. As treatment advances, the control of stimuli is fades gradually, except avoiding gambling friends. Recovering gamblers are also encouraged to meet with a financial planner, to cancel all credit cards, and to turn over control of money to another person. Self-exclusion from gambling venues can be an adjunct to treatment (Nelson, Kleschinsky, LaBrie, Kaplan, & Shaffer, 2010).
Exposure with response prevention is focused on making patients experience the desire to gamble and teach them how to resist it in a gradually more self-controlled way. The aim of systematic exposure to cues and situations of risk is to make the cues lose their power to induce urges and gambling behavior. If responses are prevented or controlled, the stimulus-response relationship will weaken. In addition, patients are taught alternative strategies to cope with their increased anxiety. This type of therapy is designed to deal with cravings and urges for gambling by increasing confidence in the ability for self-control (Echeburúa, Báez, & Fernández-Montalvo, 1996). According to the meta-analysis of Pallesen, Mitsem, Kvale, Johnsen, and Molde (2005), interventions involving developing relaxation skills, exposure to gambling cues, and direct behavioral action are effective in improving gambling urges, time and money spent, and abstinence. In addition, behavioral change is related to cognitive change after treatment.
Cognitive therapy aims to help patients challenge and overcome irrational thoughts that are believed to initiate and maintain the undesirable behavior. Patients are taught to be aware of the link among thoughts, behavior, and emotion. Many patients do not understand the concepts of probability and randomness, believing that they can exert some control over whether they win or lose. Treatment typically involves teaching patients strategies to correct their erroneous thinking by providing corrective information through education, logical discussion, or behavioral experimentation. If the erroneous perceptions and understanding of randomness in the gambler can be corrected, then the motivation to gamble should decrease dramatically. Cognitive therapy also aids gamblers in coping with urges to gamble, managing negative emotions and training in problem solving techniques (Ladouceur et al., 2001).
The more recent randomized clinical trials have focused on combined cognitive and behavioral approaches (CBT) (cognitive correction, problem solving training, and social skills training) (Jiménez-Murcia et al., 2012; Petry & Roll, 2006). Both individual and group CBT appear effective for reducing gambling. Anyway, more randomized clinical trials with bigger samples are needed to confirm the effectiveness of CBT for problem gambling (Smith, Dunn, Harvey, Battersby, & Pols, 2013).
Motivational enhancement therapy
Another approach adopted to help problem gamblers focuses on the use of short-term brief motivational enhancement therapy (MET) and telephone counseling, mailed self-help workbooks, and online resources. Brief treatment is defined as that using less professional resources or time (four or fewer sessions and sometimes one single session) than usual face-to-face interventions (typically, six to twelve sessions of therapist contact). This therapeutic modality may be an important innovation to helping people with gambling problems who fail or refuse to seek treatment in traditional therapeutic settings and may enhance patients’ sense of control over their own recovery. Motivational interviewing (MI) is often a 50-minute face-to-face or telephone session that addresses the principles of MI used to build commitment to change (Yakovenko, Quigley, Hemmelgarn, Hodgins, & Ronksley, 2015).
The MI focuses on patient’s intrinsic motivation for change and on patient’s strengths to enhance self-efficacy. This approach has proven to be effective in the short term, at least with those with less severe gambling problems (Diskin & Hodgins 2009; Hodgins, Currie, Currie, & Fick, 2009; Yakovenko et al., 2015).
A combined motivational interviewing and CBT program applied in group or individual format, or even adapted to a web-based format (Carlbring & Smit, 2008), can improve GD behaviors, as well as gambling correlates. Moreover the addition of motivational interviewing to CBT can reduce treatment attrition and improve outcomes (Wulfert, Blanchard, Freidenberg, & Martell, 2006).
However, these motivational approaches, which are more attractive to gamblers and may result in an increase of treatment seekers, cannot be so effective with severe individuals with GD or patients with comorbid pathology. Further research is required to determine the effects of MI treatment over time and the efficacy of these programs when compared to more established CBT. Besides, the efficacy may vary based on target population (severity of pathological gambling, presence of comorbidity, etc.) and on the follow-up period after the intervention (Yakovenko et al., 2015).
Self-help groups
Gamblers Anonymous (GA) is the primary self-help group focused on an abstinence-based treatment program. GD is conceptualized as an illness which can be arrested but never cured, so people affected by this problem have a permanent predisposition for losing control over their gambling.
The therapeutic rationale for GA is that the 12-steps to recovery will lead gamblers to attain abstinence. The group format is intended to provide a sense of common purpose and understanding, emotional and spiritual support, and hope. Anonymity allows for members to feel safe in sharing openly with other members (Hodgins & Holub, 2007).
The efficacy of GA has not been demonstrated in controlled studies. Relapse rates tend to be quite high. Attrition rate is also high. In some studies people attending GA have better gambling outcomes than those who do not, even though they are engaged in professional treatment concurrently (Petry & Roll, 2006).
The therapeutic effectiveness of GA has also been explored with respect to participation by the gambler’s partner. There is a trend for higher abstinence rates for gamblers whose partners are present at meetings compared with gamblers whose partners do not attend.
There is a particular need for studies of the role of GA in recovery and treatment outcomes. A recent study found that there were not any differences on key gambling variables (e. g., frequency, abstinence rates, money wagered) at 12 months between a program of CBT and 12-step therapy (Toneatto & Dragonetti, 2008).
Treating comorbid gambling disorder and severe mental disorders
Treatment of gambling disorder with affective and addictive mental disorders
There are several studies on the efficacy of treatments when there is dual disorders, especially between GD and mood disorders or alcohol/substance abuse. Psychological treatments effective in treating comorbidity between GD and depression are CBT and imaginal desensitisation plus motivation interviewing (Dowling et al., 2016).
Pharmacological treatments, such as opioid antagonists (Grant, Kim, Hollander, & Potenza, 2008), memantine, that was associated with diminished gambling and improved cognitive flexibility (Grant, Chamberlain, Odlaug, Potenza, & Kim, 2010), citalopram (Zimmerman, Breen, & Posternak, 2002), and sustained-release lithium for bipolar spectrum disorders (Chaim, Nazar, Hollander, & Lessa, 2014; Hollander, Pallanti, Allen, Sood, & Rossi, 2005) may reinforce psychological therapy.
On the other hand, psychological approaches may be effective in treating comorbidity between GD and alcohol/substance abuse: CBT, motivation interviewing, Internet delivered self-help CBT, 12-step therapy, solution-focused therapy, and dialectical behavior therapy (Dowling et al., 2016). In this therapeutic context, there are also positive results combining different approaches, such as MET + CBT (Petry, Rash, & Alessi, 2016).
Treatment of gambling disorder with schizophrenia
There are higher rates of pathological gambling in schizophrenic populations (between 4.7% and 10%) than in the non-schizophrenic population (1-5%) (Dowling et al., 2015; Haydock, Cowlishaw, Harvey, & Castle, 2015). These patients also have greater alcohol use severity, higher depression scores, and more outpatient mental health care utilization.
Apart from three case reports (Borras & Huguelet, 2007; Potenza & Chambers, 2001; Shonin, VanGordon, & Griffiths, 2014), there is only one controlled trial that tested the clinical effectiveness of a cognitive-behavioral program specifically adapted for individuals with GD with chronic schizophrenia, with post-treatment and 3, 6, and 12-month follow-up assessments. Adaptation of CBT for these individuals dually diagnosed with GD and chronic schizophrenia took into account several aspects: The active role of the therapist to help patients fulfil the self-reports; the presence of a co-therapist (a family or staff member) in order to enhance motivation for treatment, to encourage patients to carry out in vivo exposure tasks and to check information provided by patients; and the implementation of the program in the stabilization phases of the schizophrenia. This modified CBT (stimulus control and gradual in vivo exposure with response prevention) has proven to be an evidence-based psychosocial intervention for patients with these dual disorders (Echeburúa, Gómez, & Freixa, 2011).
In this study, individuals dually diagnosed with GD and chronic schizophrenia have benefited from medication and supportive psychological treatment to cope with GD. Thus, the improvement rate in the experimental group was 73.9% (with all patients being treatment completers), versus 19% in the control group at the 3-month follow-up.
Predicting relapse in GD in individuals with chronic schizophrenia after treatment can be useful in targeting patients for aftercare services. The therapeutic failure rate was 43% and it was associated to the age of first episode of schizophrenia, the number of episodes, and the age of onset in gambling behavior (Echeburúa, Gómez, & Freixa, 2017).
Future challenges
Only a small proportion of the patients who are suffering from GD (about 6%) seek formal treatment. Natural recovery from problem gambling can occur in about 35%, but most individuals with GD report a chronic course, with symptom severity fluctuating over time (Grant & Odlaug, 2012).
For individuals with GD, treatment compliance is an issue because they are often ambivalent about giving up their gambling and altering ineffective long-standing patterns of coping. Some people do not seek treatment, some drop out after one or two sessions and some can decide to terminate treatment only after a few weeks. Motivational enhancement therapy, behavior contracts and flexible treatment goals might improve treatment compliance.
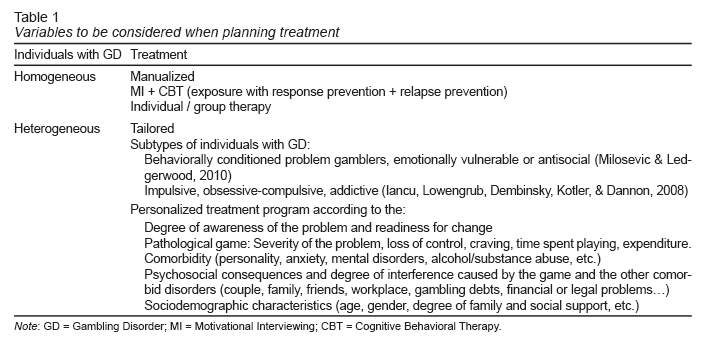
Interventions should be tailored to the needs of the patients. Substantial progress has been made in understanding the treatment of this disorder, but there is not yet research basis for matching patients to treatments according to different characteristics (e. g., subtypes of gamblers, different type of gambling or comorbid disorders). Table 1 shows some variables that could be considered in order to plan the treatment in an individualized way.
In conclusion, a combination of individual, family and group therapy may be the best option, although individualization should be emphasized. Medication (e. g., ISSRs) may be needed to treat associated anxiety or depression. Anyway, our understanding of Internet gambling is still quite limited. There is no evidence-based research for treatment options regarding this topic.
Discussion and conclusion
Both individual and group CBT appear to be effective in the treatment of GD and its correlates (Gooding & Tarrier, 2009). Group therapy is not only just cost effective; it also enables gamblers to learn from and support each other. Individual therapy may be more suitable for those who prefer discussing life events on a one-to-one basis (Oei, Raylu, & Casey, 2010).
Virtual counseling (Internet or computerized therapy) is another treatment option for individuals with GD who may be reluctant to enter individual or group therapy.
Gambling studies should focus particularly on treatments that have manual-guided treatments. Poor specification of the therapeutic methods used hinders the replication of successful programs. Not only do therapist’s manuals guide interventions, but they also facilitate the clarification of the specific contribution of particular treatment components.
Gambling behavior should be routinely investigated as part of all psychiatric assessments. Taking note of behaviors consistent with GD in individuals with severe mental disorders ‒for example, frequent missed appointments, poor medication adherence, and financial or legal problems‒ may be very helpful. Honest reporting of actual gambling is most likely to occur if the clinician establishes a nonjudgmental therapeutic alliance when assessing a patient who may have a co-occurring addiction (Green et al., 2007).
Pharmacotherapy is not the primary treatment for GD; however, patients with dysphoria should be evaluated for antidepressant medication. Family therapy may be indicated in the presence of extreme family estrangement; and substance abuse counseling may be necessary for those whose addictive behavior also includes alcohol or other drug abuse. Inpatient programs for individuals with severe gambling disorder, with comorbid disorders or attempted suicide (or suicidal ideation), may be also useful (Grant & Odlaug, 2012).
There is growing evidence for the effectiveness of psychosocial interventions, such as motivational interviewing (short in duration, easy to be administered, and cost-effective) and cognitive-behavioral therapy to cope with specific needs of people with dual disorders (Yakovenko et al., 2015). However, there are serious implementation barriers related to service organization, training and the difficulties of engaging people with a severe mental disorder in treatment (Abou-Saleh, 2004).
Programs that combine pharmacotherapy and psychosocial treatments for GD into a single comprehensive package are most likely to have good treatment outcomes, at least with regard to treatment retention.
Finally, since the population of mentally ill individuals with GD is heterogeneous, it would be interesting to evaluate a patient-treatment matching strategy intended for these dual-diagnosed patients (Chen, Barnett, Sempel, & Timko, 2006).