Background
To date, a growing body of research has distinguished between two profiles within the symptomatology developed after undergoing a traumatic experience: post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (CPTSD) (Busuttil, 2009; Karatzias et al., 2017; Lansford, Dodge, Bates, Crozier, & Kaplow, 2002; Taylor, 2006). The latter is caused by multiple or chronic exposure to one or more forms of interpersonal trauma or complex trauma (abandonment, betrayal, physical aggression, sexual assault, threats to bodily integrity, coercive practices, emotional abuse, witnessing violence and death), which causes a subjective experience marked by feelings of anger, betrayal, fear, resignation, defeat, and/or shame (Van der Kolk, 2005). These events are common in childhood and adolescence, their repercussions continuing into adulthood, where they have a strong impact on the psychosocial functioning of those who experience them (Cook, Blaustein, & Spinazolla, 2003; Felitti et al., 1998). Research has shown that these early stressors generate neurobiological sequelae in children (Bremner, 2003; Van der Kolk, 2003), and when complications arise, they may cause health problems (Goldsmith et al., 2012), substance abuse and/or psychiatric disorders, in both children and adults (Anda et al., 2006; Anda, Butchart, Felitti, & Brown, 2010).
Although CPTSD was previously included within the category of unspecified extreme stress disorder (Disorders of Extreme Stress Not Otherwise Specified, DESNOS; Pelcovitz et al., 1997), the current Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-V); American Psychiatric Association, 2013) does not include this specific problem. The closest diagnosis would be PTSD, although this is restricted to a very limited number of symptoms and contexts, since it has been shown that CPTSD also includes the following symptomatology (Herman, 1992; López-Soler, 2008): a) difficulties in the regulation of affective impulses; b) alterations in attention and consciousness, dullness, slowness of processing, difficulties in attention and concentration, amnesia, dissociative episodes, and depersonalization; c) problems of self-perception, a chronic sense of guilt, and personal responsibility accompanied by feelings of intense shame; d) alterations in the perception of the abuser (including acceptance, dependence, and incorporation of his or her belief system); e) conflicts in relationships with others, marked by difficulty in trusting and being intimate, development of strong feelings of vulnerability and danger when they engage in new affective relationships; f) somatization and/or medical problems; g) persistent changes in the system of meanings.
The World Health Organization (WHO) has proposed the inclusion of CPTDS as a new nosological entity within the eleventh edition of the International Classification of Diseases (ICD-11), due to be published shortly. Thus, CPTSD would not only be defined by PTSD symptoms, but also by the disturbances detailed above and associated with a complex trauma (Cloitre et al., 2014). Accordingly, it is postulated that the therapeutic approach should take into account the differences between the two presentations of the disorder and address the particular complexity characterizing CPTSD.
Extensive literature exists on evidence-based psychological treatments, which are therefore effective for PTSD in both the adult (Blankenship, 2017; Cusack et al., 2016) and child population (Dowd & McGuire, 2011). The two approaches include cognitive behavioral therapy (CBT), prolonged exposure therapy, and eye movement desensitization and reprocessing therapy (EMDR), accompanied by pharmacological treatment (National Center for PTSD, 2016). However, it remains to be seen whether these interventions will be able to address the symptoms of CPTSD equally effectively or whether treatments should incorporate specific components in order to address the characteristics of this specific type of disorder. For this reason, the purpose of this study was to evaluate the effectiveness of psychological therapies in reducing CPTSD symptoms in adult and child populations. Given the characteristics that distinguish the symptoms of CPTSD, this study undertook a qualitative systematic review of the studies describing treatment for CPTSD in order to demonstrate their empirical effectiveness.
Method
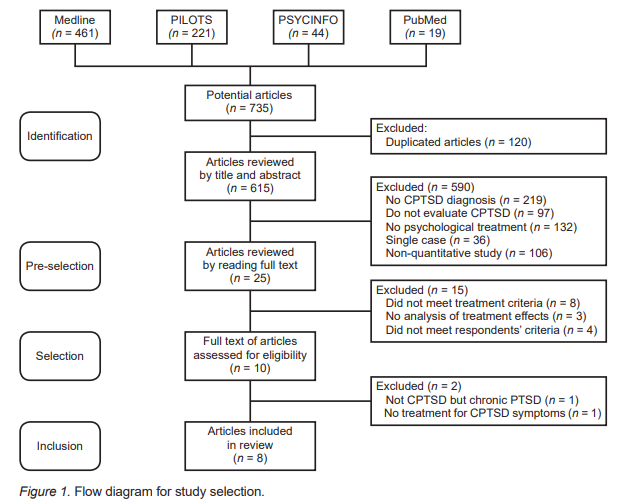
A qualitative systematic review of the literature following Perestelo-Pérez (2013), Higgins and Green (2011), and the recommendations of the PRISMA publication guide (Moher, Liberati, Tetzlaff, & Altman, 2009) was conducted. The electronic search, undertaken in May 2017, using the Medline, Pilots, Psycinfo, and Pubmed databases, was limited to documents in English and Spanish, full-text journal articles, human studies and publications on clinical trials, randomized control trials, and validation studies. It was not restricted to a set period of time in order to ensure the collection of all the articles related to the treatment of this set of symptoms given its specificity. The terms used were: Complex trauma OR complex PTSD OR Complex post-traumatic stress symptoms OR Unspecified external stress disorder AND Psychological treatment OR Psychological intervention OR Psychological therapy AND Effectiveness OR Efficacy.
Based on the aforementioned search strategy, 735 potentially eligible articles were identified by title, 120 of which were duplicated. The remaining 615 were independently reviewed by three assessors in two stages (pre-selection and selection). In the pre-selection, abstracts of all 615 articles were analyzed and those that met the following criteria were chosen for a reading of the full text: a) having a sample with a CPTSD diagnosis; b) having made an evaluation of the symptoms of this disorder; c) have provided treatment; d) being a study with an N > 1, and e) having quantitative statistical analyses. Twenty-five articles were selected on the basis of these criteria.
Following Cochrane’s recommendations for the systematic review of interventions (Higgins & Green, 2011), during the reading of the full texts of the articles, also independently carried out by the three reviewers, studies based on the following criteria (Table 1) were chosen. As far as the type of study is concerned, a higher score was given to articles involving a randomized clinical trial, which made it possible to control for selection bias. Three criteria were taken into account regarding the type of respondents: a) diagnosis (specification, according to a valid, reliable diagnostic system, with measures to guarantee this); b) comorbidity with other pathologies (in order to ensure the comparability of studies based on the characteristics of the sample to prevent selection bias; the presence of a second diagnosis or another type of psychological and/or physical problem would affect the comparison and the effects attributable to psychological treatment); and c) medication (also in order to control for performance bias, since the effects of treatment may be different when it interacts with pharmacological effects). Lastly, the type of intervention was also assessed on the basis of three criteria: a) measurement of treatment effects (in order to control for detection bias, considering how treatment results were determined in each study); b) replicability (providing sufficient details of the intervention to ensure replication); and c) follow-up (for the purpose of controlling attrition bias not only in immediate results, but also in the medium- and long-term results available).
Their score was estimated according to the degree of compliance and quality in relation to the various characteristics the articles showed within each criterion. The higher the methodological quality, the higher the score assigned. The scores given ranged from 0 (when the criterion in question was not met) to 2 (when higher quality guarantees were met). In order to ensure the quality of the potentially eligible articles, it was considered that, for each of the seven criteria, the article should obtain at least half the maximum score (in other words, one point), hence the score of seven points as the cut-off point for the selection of the articles.
Nevertheless, it was not essential to obtain one point in each criterion. In these cases a lower score in one criterion was offset by a higher score in another one. As can be seen from Table 1, only in the case of the criterion relating to the measurement of treatment effects was it necessary to obtain at least one point, since this was considered essential for the purpose of the review. Papers failing to obtain a minimum score of seven points, regarded as the cut-off score, were excluded from the final review.
A pooling session was subsequently held to agree on the scores given to each paper. As a result of this process, 14 of the 25 selected studies were excluded since they failed to achieve the minimum score required (obtaining between 3 and 5.5 points), while three other studies were ruled out for the following reasons: they addressed the issue of chronic, non-complex PTSD, presented a treatment program for abusive parents and abused children, or described an intervention performed on patients with psychiatric disorders admitted to a mental health unit.
Lastly, the following information was extracted from each of the selected articles: authors, characteristics of the sample (sex, age, size), variables evaluated, and evaluation instruments used, name and features of the psychological treatment used, number, frequency and duration of sessions, format (individual or group), and duration of treatment and follow-up, statistical analysis of the data collected, and treatment effects (taking into account the variables evaluated and CPTSD symptoms).
Results
As a result of this procedure, eight articles were identified that met the inclusion criteria to undertake the review, with scores ranging from 7 to 10. Figure 1 shows the process of selecting the studies. It should be noted that these papers were published between 2003 and 2014. The characteristics of the samples of the studies reviewed are described and, subsequently, the components of the treatments, with a distinction being made between studies performed either on adults or children.
Table 2 summarizes the main characteristics of the eight studies selected, including the authors, sample size, average age and standard deviation of the latter, gender distribution in percentages, and psychological treatment given to participants, together with sessions held and the main results of the latter.
The size of the samples analyzed ranged from 10 to 153 patients, recruited through various mental health care systems. Participants were aged between 6 and 55, with an average age of approximately 29. Four of the studies had mixed samples, while the majority had a higher percentage of female participants. The traumatic events suffered were mainly interpersonal traumas with some type of abuse (physical, sexual and/or emotional) in childhood, adulthood, or in both, with sexual abuse being present in all the studies. They had also evaluated traumatic events, PTSD, or CPTSD symptoms (using different instruments), and specified that the respondents had met the diagnostic criteria for both disorders. The respondents also had a diagnosis of comorbidity in addition to CPTSD (such as depression).
The psychological treatments used in the different studies included a variety of approaches: CBT and prolonged exposure, EMDR, sensory learning, and other specific approaches for the treatment of children. Four of the five studies conducted with adult samples were randomized controlled trials with a control group, whereas the fifth one did not randomize participants to treatment conditions. Of the three studies conducted on infant-youth samples, two were clinical studies without a control group and the third included a non-randomized control group. The results are detailed, distinguishing between the two types of population.
Results of studies conducted
on adult populations
The group treatment undertaken by Dorrepaal et al. (2013) consisted of 20 two-hour sessions. Psychoeducation on symptoms of the disorder, cognitive restructuring of dysfunctional beliefs, management of guilt, shame, anger and distrust, and assertiveness training were provided. In comparison with the usual treatment (not specified by the authors), this treatment achieved a decrease in PTSD symptom scores in the pre-post-treatment comparison; 64% of patients failed to meet CPTSD criteria post-treatment, increasing to 78% at six-month follow-up. Resick, Nishith, & Griffin (2003) compared a 12-session cognitive restructuring intervention with nine prolonged exposure sessions. The results failed to show the superiority of one technique over another, with significant differences being obtained in both cases in the symptoms of the disorder when comparing pre-, post-treatment and follow-up scores. Prolonged exposure (in imagination and live) was also used in the intervention of between 9 and 12 sessions undertaken by Feske (2008), preceded by psychoeducation and training in diaphragmatic breathing. The data indicated that prolonged exposure was significantly more effective than counseling in reducing symptoms of the disorder in both post-treatment (F = 8.54, p = .009, d = 1.19) and follow-up (F = 7.56, p = .013, d = 1.20).
Kaiser, Gillete and Spinazzola (2010) used a sensory learning program based on the Bolles (2001) proposal, which employs a trochoidal movement table, a computerized light instrument, and an acoustic training game for the purpose of creating interactions between the visual, auditory, and vestibular systems to bring about improvements in sensory integration and adaptive body responses. It produced significant improvements in various CPTSD symptoms between pre- and post-treatment in self perception [t (10) = 2.341, p = .02] and alterations in traumatic meaning [t (10) = 2.064, p =. 04] variables, and between post-treatment and follow-up in the emotional regulation variable [t (8) = 2.391, p = .03].
In turn, Sachsse, Vogel, & Leichsenring (2006) delivered specific, trauma-oriented psychodynamic treatment based on the therapy described in the imaginative psychodynamic trauma therapy (IPTT) manual (Reddemann, 2004), adding two EMDR sessions a month (Shapiro, 1995). They obtained significant improvements between pre- and post-treatment in dissociation [t (75) = 3.19, p = .05, d = .44] and avoidance symptoms [t (75) = 3.83, p = .01, d = .77], compared with the scores of the control group that received the usual treatment (not specified), which remained at one year follow-up.
Results of studies conducted
on child/youth populations
Lanktree et al. (2012) provided structured, multimodal treatment also based on the cognitive-behavioral and trauma-focused approach, which included aspects such as psychoeducation, training to improve self-control, stressor identification, controlled exposure to traumatic events, and social skills training in all contexts. The whole intervention period was accompanied by games and group and family activities. The intervention significantly reduced symptoms associated with CPTSD (F = 59.20, p < .001, η2 = .29).
Jarero, Roque-López, and Gómez (2013) undertook two group EMDR sessions together with integrative group treatment (EMDR-IGTP), based on the program developed by Jarero and Artigas (2009), to which they added six individual EMDR sessions, in keeping with the procedure designed by Shapiro (2001). In addition, psychoeducation was provided for respondents’ families, who were also taught communication and empathy skills, as well as mindfulness techniques. Analysis of the effect of time showed a significant decrease in symptoms of the disorder between pre- and post-treatment, as well as between post-treatment and three-month follow-up (F1,33 = 259.27, p < .001).
Lastly, Kagan, Henry, Richardson, Trinkle, and LaFrenier (2014), developed a group program for children and adolescents focused on emotional regulation, affective social support, and life history integration to build resources and resilience skills. The content of the sessions was based on sharing the feelings and emotions experienced, with therapy focusing on improving self-control, together with mindfulness exercises for stress reduction. The therapy produced a significant reduction in symptoms between pre-treatment measures and follow-up at six months in total PTSD symptom scores (29.4 vs. 20.6, t = 2.93, gl = 18, p = .009). A significant reduction in symptoms and emotional and behavioral problems between pre-treatment and follow-up at nine months was also observed (68.1 vs. 60.2, F = 6.61, gl = 3, η2 = .38, p = .001).
Discussion and conclusion
The purpose of this study was to conduct a qualitative systematic review, based on the recommendations of the PRISMA publication guide (Moher et al., 2009), on the effectiveness of treatments used to address CPTSD. The results of these studies showed that significant improvements were achieved in CPTSD symptoms, although the components and structure of the interventions were not necessarily the same. It cannot therefore be said that any particular intervention is more effective than other treatments for this condition.
In general, and based on the articles selected , the work undertaken to date to treat CPTSD includes interventions designed not only to alleviate its symptoms, but also the manifestations that complicate and cause the severity of this disorder. The studies reviewed agreed on the need to address alterations in emotional regulation, difficulties in maintaining attention and awareness, problems of self-perception and guilt, negative cognitions, difficulties with others, and somatization and/or associated medical problems.
Although the interventions analyzed yielded positive results, the different characteristics of the samples (with widely varying sizes, different ages, and the presence of various comorbid disorders with CPTDS), the variety of treatments and techniques used and the structure of the intervention (format, duration, and frequency) hamper comparison across studies and the choice of a set therapeutic modality. However, three of the studies conducted on adults (Dorrepaal et al., 2013; Feske, 2008; Resick et al., 2003) and one of those undertaken on children (Lanktree et al., 2012) were based on the cognitive-behavioral approach, in which cognitive restructuring with prolonged exposure (Resick et al., 2003) or without it (Dorrepaal et al., 2013) was used, together with exposure to trauma as the main technique (Feske, 2008; Lanktree et al., 2012).
In the case of adults, the main treatment components were: psychoeducation (Dorrepaal et al., 2013; Feske, 2008), cognitive restructuring techniques (Dorrepaal et al., 2013; Resick et al., 2003), and exposure techniques (Feske, 2008; Resick et al., 2003; Sachsee et al., 2006). Kaiser et al. (2010) implemented a sensory learning program while Sachsse et al. (2006) complemented exposure with EMDR sessions and imaginative psychodynamic therapy for trauma. Data from these papers show that these treatments also affected depression, anxiety, and anger scores and the general level of distress. Resick et al. (2003) specifically reported a decrease in symptoms related to intrusions, avoidance, dissociation, and sexual concerns. Through their intervention, Kaiser et al. (2010) managed to improve self-regulation, self-perception, and alterations of meaning, by using the Sensory Learning Program, while Sachsse et al. (2006) declared that specific psychodynamic treatment oriented towards trauma led to improvements in dissociative symptoms, and an improvement in overall and behavioral functioning. Thus, although the results derived from these studies may point to the fact that psychoeducation, cognitive restructuring, and exposure could be effective techniques for the CPTSD treatment, the differences in the design of the treatments and the characteristics of their application make it impossible to say what the exact structure of this intervention should be. More research is therefore required in this respect.
Regarding the results obtained in the child and adolescent population, findings are diverse and do not point to a single intervention protocol, although emotional regulation was a common feature of the three studies reviewed. Eye movement desensitization and reprocessing, together with the integrative group treatment protocol (EMDR-IGTP) designed by Jarero et al. (2013), produced an increase in mastery and confidence regarding traumatic memories in the children in whom it was implemented. The Real Life Heroes Treatment program (Kagan et al., 2014) was also effective in improving the symptoms of internalization, externalization, and overall behavior of the children who took part in this program. In the study by Lanktree et al. (2012), reductions in levels of anxiety, depression, dissociation, and sexual concerns were achieved through the use of integral treatment for complex trauma. The dearth of papers with methodological control, together with the various therapeutic procedures used in the studies analyzed, once again demonstrates the need for further research in this field.
Given the range of procedures, samples, evaluated psychological variables and components of the interventions, it is only possible to affirm that psychological intervention is undoubtedly necessary and useful in this problem in both child, adolescent and adult populations. It is not possible, however, based on the evidence available after this review, to identify the treatment of choice for CPTSD. Only psychoeducation, cognitive restructuring and prolonged exposure, which have traditionally been used in PTSD treatment (National Center for PTSD, 2016), are likely to be effective treatments in the adult population. However, as indicated at the beginning of this paper, CPTSD treatment requires addressing other psychological variables that may require other specific techniques for this disorder. In the case of the child and adolescent population, the absence of common therapeutic components is evident, which makes it difficult to opt for a specific treatment.
It is essential to point out the limitations of the review undertaken. These include the low number of studies analyzed, since only eight of the potentially eligible papers met the inclusion criteria established in the present review. Moreover, despite following Cochrane’s recommendations for the systematic reviews of treatments, the methodology used to select them was based on an arbitrary cut-off point for the selection of articles. Although this proved useful to reach an agreement on the articles to be included in the review and ensuring that they were of sufficient quality, a different cut-off point would have enabled more papers to be reviewed. However, the excluded articles had scores far below this range, showing that they were of poorer quality. At the same time, not all the selected studies were randomized controlled clinical trials, indicating the presence of methodological biases. As mentioned earlier, the samples in the various papers were extremely heterogeneous. It is also worth mentioning the absence of a follow-up after treatment in some studies, as a result of which the data on the long-term maintenance of the therapeutic effects achieved are not conclusive either.
Despite these constraints, as far as we know, this is the first systematic qualitative review designed to analyze the state of the art of effective therapies for the treatment of complex posttraumatic stress. Its results highlight the need to undertake studies with better methodological control, regarding sample selection and diagnostic criteria (traumas caused by abuse or maltreatment), the psychological variables the treatments seek to address (which should distinguish PTSD symptoms from those of CPTSD), and control of pharmacological treatment (symptoms for which the effects on them are prescribed). There is also obviously a need to design research with a control group. In the cases where control groups exist, the components of the usual treatment with which the comparisons are made should be clearly specified. We believe that the specificity and complexity of this disorder, which has severe effects on those suffering from it, requires effective interventions to address its particular characteristics.