Background
Anorexia nervosa (AN) is a complex disorder. Its clinical course is highly variable and the reasons why some individuals evolve towards chronicity, whereas others achieve remission and recovery, are not yet clear. Thus, preventing patients from becoming resistant to treatments is fundamental since unfortunately, an important percentage of them tend to develop a severe and enduring disorder, and because relapse is highly associated with psychiatric comorbidity, poor prognosis, and serious medical consequences due to malnutrition (Treasure, Stein, & Maguire, 2015).
The contemporary view on the therapeutics of anorexia nervosa supports the benefits of involving the family in the treatment, and over the years it has been demonstrated that better results are obtained if parents are committed to the treatment (Treasure & Cardi, 2017).
Among the current, most used interventions for the treatment of AN, we can mention the Maudsley model and the new Maudsley model, intended for the management of adolescents and adults (Rhodes, 2003; Schmidt, Wade, & Treasure, 2014); as well as the family-based treatment and the emotion-focused family therapy, both based in the transdiagnostic theory (Fairburn, Cooper, & Shafran, 2003; Lafrance Robinson, Dolhanty, Stillar, Henderson, & Mayman, 2016; Loeb, Lock, Le Grange, & Greif, 2012). Despite the great body of evidence supporting the effectiveness of these interventions, they are intended for the treatment of early stages of the disorder. Currently, therapeutic options are reduced for those individuals who begin to show signs of a severe and enduring disorder (Touyz & Hay, 2015), and they are not as clearly established as the effective treatments for initial stages.
It is complex to talk about severe and enduring anorexia nervosa (SEAN) given the lack of consensus about how to best define this population (Ciao, Accurso, & Wonderlich, 2016).
Defining SEAN has been operationalized in several different ways. Early theoretical perspectives highlighted motivational aspects such as “resistance” (Hamburg, Herzog, Brotman, & Stasior, 1989) or “refusal” (Goldner, 1989) to treatment. It has also been broadly defined placing the focus on “chronicity.” Others have defined it by chronicity (as a duration of illness greater than ten years) and clinical severity (as the point at which symptoms significantly impair quality of life (Robinson, 2009). Perhaps, currently the most comprehensive definition describes a combination of clinical severity (as the difficulty in maintaining a regular functioning), treatment failure (as failure to reach sustained improvement with previous treatments), and chronicity (Golan, 2013).
Just as there is no current consensus about the definition of SEAN, there is no agreement about what is the best way to treat it. So, given the poor response to standard treatment, the prolonged impasse, and the relapse that characterize this case, we consider this to be a disorder where early signs of SEAN are manifested.
In this article we expose the therapeutic effect of the protocol for severe and enduring cases of anorexia nervosa at relapse used at the Eating Behavior Clinic of the Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz (INPRFM, National Institute of Psychiatry). This protocol is addressed to individuals diagnosed with anorexia nervosa, and to their families; particularly their parents. In addition to the psychiatric and nutritional management administered according to treatment guidelines (National Institute for Clinical Excellence, 2004), the protocol comprehends attendance to the psychotherapeutic group for patients with anorexia nervosa, and to the psychotherapeutic support group for parents; administered separately. Group sessions are held weekly for 2 hr., with an open format and there is not a determined number of sessions conforming this intervention. In this format, both veteran and new individuals co-participate. The therapeutic intervention is administered by one psychotherapist and two co-therapist expert in eating disorders. It combines a psychodynamic style with cognitive analytical and supportive psychotherapy interventions. The protocol was developed upon the base of systemic therapy theoretical foundations, which have widely described the influence of the family on predisposing and maintaining factors of the disorder (Bruch, 1978; Minuchin et al., 1975; Rausch Herscovici & Bay, 1990; Selvini-Palazzoli, Cirillo, Selvini, & Sorrentino, 1998).
Here we present an emblematic case, showing the importance of getting the parents involved in the treatment of anorexia nervosa. This is the case of K, a young woman diagnosed with anorexia nervosa with clinical signs of a severe and enduring disorder, who achieved clinical improvement after her parents, but nor her, were administered an intervention with group family psychotherapy.
Case report
Patient information
We present the case of K, a 23-year-old woman who showed up at the Eating Behavior Clinic (EBC) from the INPRFM six years ago, accompanied by her mother and father. Upon admission she was single, she had no romantic partner, and she was studying high school. Her socio-economic status was medium.
Reason for consultation
She was referred to psychiatric attention by the high school psychologist, given her poor academic performance and because of recurrent behavioral problems with her schoolmates and with authority. It is noteworthy that they were K’ parents who sought psychiatric attention on the recommendation of the school psychologist, but not because of the symptoms of the eating disorder.
Family and psychosocial history
They presented a familiar dysfunctional style characterized by an overprotective mother and a symbiotic relationship of the mother-daughter dyad. The father was emotionally detached from the family, and his roll was that of an economic provider. K’s sister is eight years younger than her. K referred she had felt jealous from her sister since she was born and so their siblings’ relationship has been troubled over the years. K’s parents presented a dysfunctional relationship characterized by lack of communication, frequent conflicts, and infidelity of the father; they have separated twice because of violence problems among them.
K’s relationship with her family was characterized for showing disruptive and aggressive behavior towards her parents and sister. At school, she had a long history of problems such as being abusive with her peers, showing defiant attitudes towards authority, and being frequently absent from classroom and school. Regarding social functioning, K referred having no lasting friendships. She also said she had never been able to keep a romantic relationship.
As for the nuclear family of K’s mother, her older sister had cerebral palsy, which caused K’s mother to function as mother of her siblings, while K’s grandmother took care of the sister with the disability. She described that both her siblings and her parents had always had problems controlling their impulses. K’s mother reported having an eating disorder during adolescence. She has also had multiple episodes of depression and anxiety, and is currently under pharmacological treatment.
In reference to the nuclear family of K’s father, he reported that everyone in his family, including him, has had multiple stories of both, interpersonal and couple conflicts due to the fact they have had both physical and verbal violent behaviors. K’s father has been an alcohol user since he was 18 years old. He is currently diagnosed with depression and is under pharmacological treatment.
Clinical findings
Upon admission, K presented a BMI of 16.0 ‒indicative of malnutrition‒, frequency of vomiting of 70 a week, compulsive exercise, self-injuries, risk behaviors, such as frequent casual sex and substance abuse, and depressive symptoms. She also showed distortion and dissatisfaction with her body image, and refered perceiving herself as “big and fat.” As for her global functioning, she presented lack of healthy coping strategies, interpersonal troubles, difficulties completing high school, and serious defiant and violent behavior towards her parents and other authority figures.
Her eating disorder started when she was 12 years old. The first behavior she identified was the change in the way she ate, decreasing the intake of everything she considered had excess calories, such as sweet food, flour, fat, and cereals. Later she began restricting the intake of proteins until she sustained a vegetarian diet. In addition, she regularly fasted and counted the ingested calories.
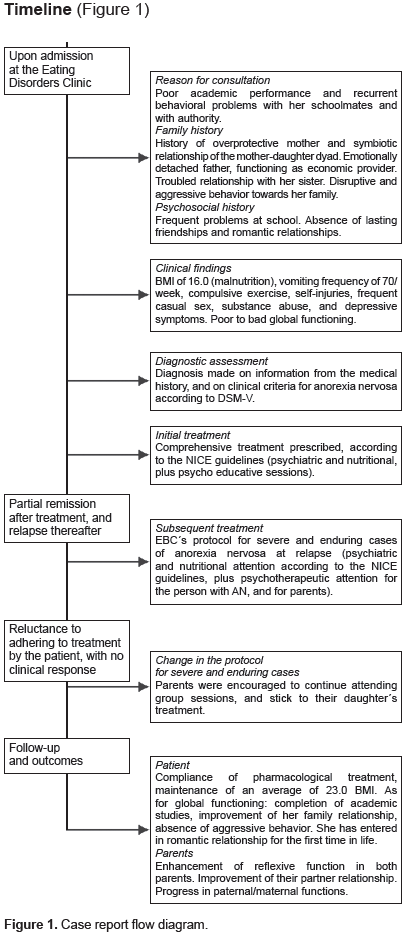
Timeline (Figure 1)
Diagnostic assessment
K was diagnosed with anorexia nervosa, binge-purgative subtype. Diagnosis was established based on information from the medical history and on clinical criteria for anorexia nervosa according to the DSM-V, assessed through a semi-structured interview by a psychiatrist expert in eating disorders.
After relapse, an expert psychiatrist made the clinical assessment, through semi-structured interview, in order to determine subsequent treatment.
Treatment history
Psychotherapy
During the first interview with the psychotherapist, K referred she had received multiple psychological treatments, with no effect at childhood, because she regularly showed aggressive behaviors and harassment towards her schoolmates, as well as lack of limits and defiant attitudes towards authority. She revealed she used to make fun and ignore the advice from all child psychologists who treated her.
Psychiatry
She had never received psychiatric treatment up to her admission at the EBC.
Therapeutic intervention along the case
Initial treatment
A comprehensive treatment was prescribed for K at the EBC, according to the NICE guidelines (National Institute for Clinical Excellence, 2004), including attention by a psychiatrist and a nutritionist, plus psycho-educative sessions. After 25 weeks of treatment, medical stabilization, decrease of vomiting frequency and compulsive exercise was achieved. However, K remained in impasse for the following three years, showing amenorrhea, and a BMI of 18.5, indicative of poor nutrition. As for behaviors such as casual sex, abusive behavior with her peers, and violent behavior towards her parents also remained unchanged. Despite the impasse, it should be noted that during those three years she presented decrease of scholar absences, of defiant attitudes towards school authority, and of substance use as well; so she was able to complete high school.
Relapse
Shortly after K finished high school she relapsed, presenting compulsive behaviors and weight loss again with a BMI of 17.5; this time she was reluctant to go on with her psychiatric treatment and her academic studies. For that reason, her parents returned to the EBC to ask for help. They referred feeling helpless and exceeded by her daughter’s attitudes, and being afraid to face a situation they did not knew how to handle.
Subsequent treatment
In this occasion, the prescription was the EBC’s protocol for severe and enduring cases of anorexia nervosa at relapse, which sustain psychiatric and nutritional treatment according to guidelines (National Institute for Clinical Excellence, 2004), and adds psychotherapeutic attention for the diagnosed individual and also for her parents. The protocol sets the administration of a weekly session of 2 hr. at the psychotherapeutic group for patients with anorexia nervosa, and the psychotherapeutic support group for the parents of those patients; delivered in separated groups.
Although K was still reluctant to continue under treatment; she agreed to attend the psychotherapeutic group under her parents’ pressure. After six sessions, she decided to stop attending the psychotherapeutic group arguing that her medical condition was much better than the condition of the other attendees to the group. She additionally said, she got worse each time she got exposed to the patients’ group.
Change in the protocol for severe and enduring cases
The protocol states psychotherapeutic attention for both the diagnosed individual and her parents. Given K’s refusal to stick to the protocol, from that moment to date, she has only attended the psychiatrist appointments for pharmacological follow-up, every three to six months. However, her parents were highly encouraged to continue attending their group sessions, and to stick to the prescriptions ordered by the psychiatrist and the nutritionist to their daughter. They did it so.
Follow-up and outcomes
At the present time, K is 23 years old and her parents continue attending the psychotherapeutic support group sessions.
In order to know the outcomes of the protocol administration, a semi-structured interview by a psychiatrist expert in eating disorders was applied to K, and clinical assessment based on expertise was adapted for K’s parents. As for the therapeutic achievements we can report the following.
In regards to K’s actual condition, she has been able to stick to the pharmacological treatment and maintain a stable and healthy BMI of 23.0 on average. As for her global functioning, she has completed academic studies at the university, she has significantly improved the relationship with her sister and her interpersonal relationships as well (for the first time she has been able to keep romantic relationships in two different occasions), and she has been able to keep under control all her risk behaviors.
In relation to K’s parents, we can say that the reflexive function of both parents has notably improved. They have referred that through the observation and analysis of the experiences shared at the group, they have been able to identify their own behavior and, consequently, modify it. Likewise, they have been able to improve their ability to observe their daughter’s behavior and, consequently, change the way they relate to her.
They have mentioned that the psychotherapeutic support group has helped them to recognize that they used to have aggressive attitudes towards K, and they understood that those attitudes were related to the anger they felt towards her. They also have been able to observe and modify the ambivalence they showed for years about their daughter’s improvement. In relation to it, they have acknowledged how for them it was more difficult to be parents of a healthy daughter than of a sick one, since in that way there was no longer someone to blame for situations such as family dysfunction or lack of money.
They have also reported the treatment has helped them improve their partner relationship. They have noted an important reduction in the conflicts related to their different points of view, and of their recurrent struggles to reach agreement and to give in to each other.
Specifically, as for K’s mother, she knows now how to set limits, which has helped her daughter to comply with pharmacological treatment and continue her academic studies. In relation to the insight arising from the group sessions, K’s mother granted having been negligent, and admitted that K suffered abuse being a child. She was also able to identify certain affections she had had towards her daughter that contributed to maintain K’s disorder; for example, giving birth at a troubled time of their marriage, or the fact that she wished a son instead of a daughter. She could also acknowledge that her daughter had not fulfilled her expectations as mother, and as a consequence she fomented a troubled relationship.
Specifically, as for K’s father, he was able to recognize how through his daughter he tried to compensate the shortcomings of his life as student involving her, against her will, at extra-curricular activities he would have liked to develop at. He could also acknowledge how his daughter’s disorder helped him to keep the mother engaged with K full time, so he could let unattended his family’s emotional needs. Therefore, he was able to go out with friends as much as he wanted, to get drunk, and be unfaithful to his wife; and even when he used to be the economic provider for the family, he used to avoid his emotional responsibility as a father and husband.
In summary, after the treatment of K’s parents at the psychotherapeutic support group, emotions, thoughts, behaviors, and global functioning were notoriously modified in a positive way, both in K and her parents, at individual and family level. Currently, K can be considered to be in remission of the symptoms she formerly presented.
Discussion and conclusion
The clinical evolution observed in this case supports the indication that group family psychotherapy is effective to treat of SEAN at relapse. We believe this is an emblematic case of the clinical application of the Eating Behavior Clinic’s protocol for SEAN since, after relapse, the patient has only attended psychiatric and nutritional follow-up consultations, and she has not received any psychotherapeutic treatment again.
Treatment guidelines for the early stages of the disorder (National Institute for Clinical Excellence, 2004) indicate the administration of cognitive behavioral psychotherapy as a required condition in order to achieve an effective modification of the symptomatology. Thus, we could expect, in late stages of the disorder, psychotherapy to be one pillar of the patient’s treatment. It is notorious that while in the case we present here such a condition did not happen, it is still remarkable that the patient’s sympotmatology is currently in remission. In saying the above, we do not try to understate the psychotherapeutic intervention that a patient should receive. On the contrary, the fact that in this case there was a modification in the patient’s condition through psychotherapeutic work with her parents, supports the idea about there is a type of family functioning that in some cases predisposes and/or perpetuates the disorder. Virtually all current interventions involve the family taking an active part in the treatment (Fairburn et al., 2003; Lock & Le Grange, 2005; Loeb et al., 2012; Rausch Herscovici, 2013; Rhodes, 2003; Schmidt et al., 2014; Treasure, Rhind, Macdonald, & Todd, 2015). This aims to empower them, to provide them with information and tools to improve their coping strategies and their understanding of the disorder, and to help them modify the ways in which they relate to each other that might be perpetuating the disorder. So, the family has become one of the focus of the treatment not because they necessarily have caused the disorder. However, the reorganization around the disorder generates dynamics that in some families perpetuate the disorder in such a way they have become a part of it (Rausch Herscovici, 2013). In relation to this, it has been described the influence of the relatives, as well as the type of close interpersonal interaction ‒crystallized through the expressed emotion (EE) construct‒, affecting the adherence to treatment and outcome of the AN. It also has been shown there is an interaction between the level of EE and the type of family intervention, so families with higher levels of EE have a better outcome with separate family therapy (the subject with AN and the parents are treated apart), compared to cojoint family therapy (Allan, Le Grange, Sawyer, McLean, & Hughes, 2018; Duclos et al., 2018; Eisler et al., 2000; Le Grange, Hoste, Lock, & Bryson, 2011; Moskovich, Timko, Honeycutt, Zucker, & Merwin, 2017; Schmidt & Treasure, 2006; Uehara, Kawashima, Goto, Tasaki, & Someya, 2001).
Regarding the findings mentioned above, we want to point out that since the late 70’s it has been described that eating disorders take place in the context of specific family dynamics driven by a set of rules in which family members tend to repeat behaviors that compromise the autonomy of other members. Thus, a maintenance circuit for those behaviors emerges and the psychosomatic symptom is self-perpetuated over time (Dawson, Rhodes, & Touyz, 2014; Lecomte et al., 2019; Liebman, Minuchin, & Baker, 1974; Pace, Cavanna, Guiducci, & Bizzi, 2015; Reich, von Boetticher, & Cierpka, 2016). This mechanism has been described as characteristic of alexithymic (Onnis & Di Gennaro, 1987) or psychosomatic families (Minuchin et al., 1975) in which the eating disorder acts as a symptom that helps the family to avoid conflict and emotional stress, or to express the conflict somatically. Systemic therapy has described how communication in these families occurs through the eating disorder, which becomes a channel needed to connect and cope with the emotional world (Minuchin, Rosman, & Baker, 1978). The dynamics displayed by these families show characteristics matching the toxic family stress, a term referring to a particular type of stress exposure that is frequent, sustained, and uncontrollable, and which occurs in the absence of buffering protective factors. From that perspective, EE may represent a form of toxic family stress, since it corresponds to maladaptive patterns of response to psychiatric illness (Peris & Miklowitz, 2015). In that sense, EE can on the one hand occur as a result of unresolved predisposing factors that act individually through attitudes such as high criticism, hostility and/or emotional over-involvement expressed by relatives of the patient with a psychiatric disorder. On the other hand, EE may become a factor that perpetuates the disorder and/or predisposes a poor outcome (Allan et al., 2018; Le Grange et al., 2011; Moskovich et al., 2017; Schmidt & Treasure, 2006).
The Eating Behavior Clinic’s protocol for severe and enduring anorexia nervosa is based in the theoretical principles and clinical application of the systemic approach proposed by Minuchin, Bruch, and Selvini (Bruch, 1978; Minuchin et al., 1975; Selvini-Palazzoli et al., 1998). This protocol focuses on the individual condition of each participant in relation to the eating disorder acknowledging that, according to systemic theory, the achievement of modifications in the behavior of each individual family member is able to elicit changes in the previous configuration of the whole system. So, one plausible reason why K was able to achieve remission, even when only her parents attended the psychotherapeutic sessions, is that the modification of the parents’ behavior was able to elicit a reorganization of the family dynamics that directly impacted the way they related to her daughter and the disorder. More technically, we may say that group family psychotherapy offered a reflective space for K’s parents, where they were able to identify what was their internal representation of their daughter, so they could understand, recognize and modify the behaviors held up by them that were perpetuating the disorder. We can also suggest that clinical application of the protocol for severe and enduring anorexia nervosa was able to stimulate reflective function (Fonagy & Target, 1997) of K’s parents. We think this was a crucial element to modify the dysfunction in the family.
Finally, through this clinical case, we have sought to strength on the notion of treating the family to manage SEAN early during relapse. We consider the protocol we used to treat this case constitutes a novel intervention for several reasons which, additionally represent strengths in our approach to this case: it addresses the need for feasible alternatives to treat anorexia nervosa in late stages, it places relapse as the opportunity to engage family into treatment, it brings back to psychotherapy the approach of systemic theory regarding family functioning in anorexia nervosa, and it sheds light on systemic therapy as a current and effective intervention for severe and enduring cases.
We consider it is necessary to extend the follow-up period in order to assess the protocol, and settle its strength and application for anorexia nervosa with early signs severe and enduring disorder. We additionally acknowledge the need of further research of this intervention through randomized clinical trials.