Introduction
The short-, medium- and long-term consequences of the COVID-19 pandemic are still to be documented. However, research on previous epidemics, and the new information that is beginning to appear, shows that fear of contagion, uncertainty, and social distancing and quarantine measures can result in mental health issues, especially for vulnerable populations. Migrants are of particular concern in this regard, as they face disadvantages in access to work, healthcare and social services beyond those of the local population, and can also be met with xenophobia and stigmatized as infection transmitters (Guadagno, 2020). Added to this, in-transit migrants, refugees and asylum seekers face particular difficulties related to the COVID-19 pandemic. On the one hand, many of them have limited access to adequate spaces to shelter in place or isolate if needed, as well as to healthcare. On the other, limitations to cross-border mobility have left many of them stranded in dire conditions, and those who were already settled have lost their sources of income without having social safety nets to fall back into. All of these conditions can put people on the move, and especially those who migrate because of violence in their places of origin, at increased risk of mental health problems (Júnior et al., 2020).
As different types of migrants experience different kinds of stressors, the prevalence of mental health problems also varies between them. In general, first-generation economic immigrants in high-income countries have a lower prevalence of mental disorders than the local population, while refugees and asylum seekers experience more mental health issues. As the reasons for fleeing their country of origin have to do with violence and other traumatic events, it is not surprising that higher levels of anxiety, depression and post-traumatic stress disorder have been documented among the latter (Fazel, Wheeler, & Danesh, 2005; Lindert, von Ehrenstein, Priebe, Mielck, & Brähler, 2009; Niemi et al., 2019). With the COVID-19 pandemic, these problems could become even more prevalent (Júnior et al., 2020).
In the past lustrum, about 400,000 Central American migrants have crossed Mexico each year aiming for the United States (Rodriguez Chávez, 2016). Members of this migration flow have diverse reasons for leaving their places of origin. Some are economic migrants in search of a better life, but an important number are fleeing criminal or state violence (Keller, Joscelyne, Granski, & Rosenfeld, 2017). In this sense, this is a mixed migration flow, mainly composed of economic migrants, but with an increasing proportion of refugees, asylum seekers and displaced population (Giorguli-Saucedo, García-Guerrero, & Masferrer, 2016). The mental health risks they face might therefore be a mixture of those of economic migrants and refugees, such as experiences of violence, and the difficulties of being in an ambiguous legal condition in which to move forward to participation in the host society is not always possible (Haas, 2017; Júnior et al., 2020; Niemi et al., 2019; Thomas, Roberts, Luitel, Upadhaya, & Tol, 2011). The needs and vulnerabilities of members of mixed flows might therefore be different from those of economic migrants, and strategies to promote their mental health are required.
Another important aspect of the experience of members of mixed migrant flows in Mexico is their being “stopped in motion” (Odgers-Ortiz & Olivas-Hernández, 2019). Previously conceived as in-transit migration, the trajectories of many members of these flows now include stays of months or even years at a time, as they are blocked by the migration containment policies of both the United States and Mexico. Thousands of these migrants wait in cities in Mexico’s northern border, either to be smuggled across the border or to apply for asylum in the United States (Torre Cantalapiedra, 2020). Moreover, thousands have been returned to the Mexican side of the border by the United States’ migration agencies to wait for the resolution of their asylum status under the program known as “Migrant Protection Protocols.” During the COVID-19 pandemic, the United States government used public health concerns as a rationale to deny entry and expedite return to Mexico of migrants, even when they are not Mexican nationals, a practice criticized by public health experts (Columbia University Mailman School of Public Health, 2020). The use of the public health discourse to justify a hardening of migration policies has forced migrants to spend months waiting in Mexico, at a time when their chances to work, as well as the resources of the organizations that usually support them, have been curtailed by the pandemic mitigation measures (Del Monte & Irwin, 2020). All of this puts the migrants livelihood at risk (Guadagno, 2020), and given their living conditions, they might also be at risk for SARS-CoV-2 infection (Bojorquez, Infante, Vieitez, Larrea, & Santoro, 2020).
An important aspect to consider is that most of the mental health issues migrants face are not pathologies (i.e., psychiatric disorders), but are better described as psychological distress arising from exposure to socially-determined, structural violence (Farmer, 2004; Niemi et al., 2019). The psychosocial framework captures this by placing mental health and wellbeing in a network of social relationships, and mental health problems as psychosocial issues that require interventions beyond those of the healthcare system. While there is no agreed definition of the term psychosocial, it is generally employed to refer to psychological or mental aspects that are inseparable of a person’s relationship with others, to the impact of socially determined circumstances on the mental health of individuals and collectives, and to actions that aim to support the psychosocial wellbeing of individuals and their families or communities. In this sense, the psychosocial framework is close to and complements the mental health framework (Inter-Agency Standing Committee [IASC], 2007; Organización Internacional para las Migraciones [OIM], 2018), when mental health is understood as a general state of wellbeing inseparable of social relationships and going “beyond the absence of mental disease” (World Health Organization [WHO], 2014). During the COVID-19 pandemic, it is precisely this network of social relationships that can be disrupted, and therefore psychosocial support becomes even more necessary.
Research on COVID-19 is still developing, and a recent position paper (Holmes et al., 2020) stressed the need to collect data on the mental health consequences of the pandemic and how they can be mitigated in vulnerable groups, including migrants. The authors of that paper argued that research on these issues should include rapid qualitative research to identify specific aspects of marginalized groups’ experience. In this article, we present the results of one such study. Our objective is to describe three main aspects: 1. the mental health consequences of the pandemic and lockdown measures among migrants living in shelters operated by civil society organizations (CSOs) in Tijuana, Mexico, during the COVID-19 pandemic; 2. barriers to access mental health care during the pandemic lockdown period; and 3. the key elements of the psychosocial support provided by CSOs that could protect migrants’ mental health during this period.
Method
Design of the study
We conducted a rapid qualitative study (Taylor, Henshall, Kenyon, Litchfield, & Greenfield, 2018) of migrant shelters in Tijuana, in April-May 2020, gathering information through interviews with seven participants who are members of shelters’ staff or involved in providing services at the shelters. We chose the rapid methodology, as it can deliver timely information regarding an ongoing situation, with results that can be useful for decision-makers.
The rapid study was part of an ongoing ethnographic study (“Trajectories of health and migration”), which began in 2019 and employs a combination of individual, semi-structured interviews with migrants, volunteers and shelter staff, and healthcare providers, as well as participant observation in shelters, to understand how trajectories of migration and health interact in the lives of migrants. As part of that study, the researchers have spent time in the shelters, volunteering and conducting interviews. Before the study began, the researchers had already conducted other research and service projects in the shelters, and shared a commitment to research as a way to make more visible the inequities experienced by migrants.
Places and participants
Tijuana is a city of over 1.6 million inhabitants at the northern border of Mexico. Lately, it has become noticeable as a place where migrants get “stopped in motion” in their journey to the United States. A recent study reported that 31 migrant shelters existed in the city, 30 of which were run by CSOs. The conditions and resources available in the shelters vary, and while all of them have running water and electricity, only two thirds have access to the internet. Health services in the shelters are scarce, with only 32% reporting having them regularly. At the same time, 68% of the shelters surveyed in that study reported that they provided some sort of psychological support to the migrants, although it was not specified which type of support (Coubès, Velasco, & Contreras, 2020).
The parent project from which research in this article came is being conducted in eight of those shelters, selected by convenience sampling, that reflect the variability of the city’s shelters in terms of the number of persons they can accommodate, the type of population they serve, their religious (or non-religious) orientation, and their material and human resources. For the rapid qualitative study, a convenience sample of persons (n = 7) who are part of the staff or collaborate with one or more of the eight shelters was selected. Participants were selected on the basis of their being closely involved with the shelters’ day to day activities, and having first-hand knowledge of the activities that were implemented in the shelters before and after the lockdown. We called potential participants to invite them, explaining the study’s objectives and methods, and asking their consent for a remote interview (online or over the phone). There were no refusals to participate. Because of previous collaborations, including the parent study, interviewees are well-acquainted with the researchers and their work.
Procedure and statistical analysis
For this article, we employed information from the seven individual interviews conducted in April-May 2020, as well as data previously obtained from interviews with migrants and participant observation as part of the parent study.
Five interviews were conducted online (through Zoom, Skype and Blue Jeans) and recorded, and two were conducted over the phone without recording (the interviewers took notes of the participants’ responses). There were no transcriptions of the interviews, so analysis was based on the recordings and notes only. The audio files and notes were only accessed by the authors of this article, and kept in password-protected computers to prevent confidentiality breaches. All three authors participated equally in interviews and analysis, listening to all interviews and reading the corresponding notes. They are all familiar with the material from the parent study. Preliminary and final conclusions from the analysis were discussed among the three of them. All three authors are female, hold PhDs and work as professors-researchers at an academic institution. All three authors have ample experience in qualitative methods and working with vulnerable populations.
The interview guide asked about the mental health issues that, according to the respondents, migrants were experiencing during the lockdown period, the actions that the shelter had taken in response, and the barriers and facilitators of that response. Interviews lasted from 30 minutes to one hour.
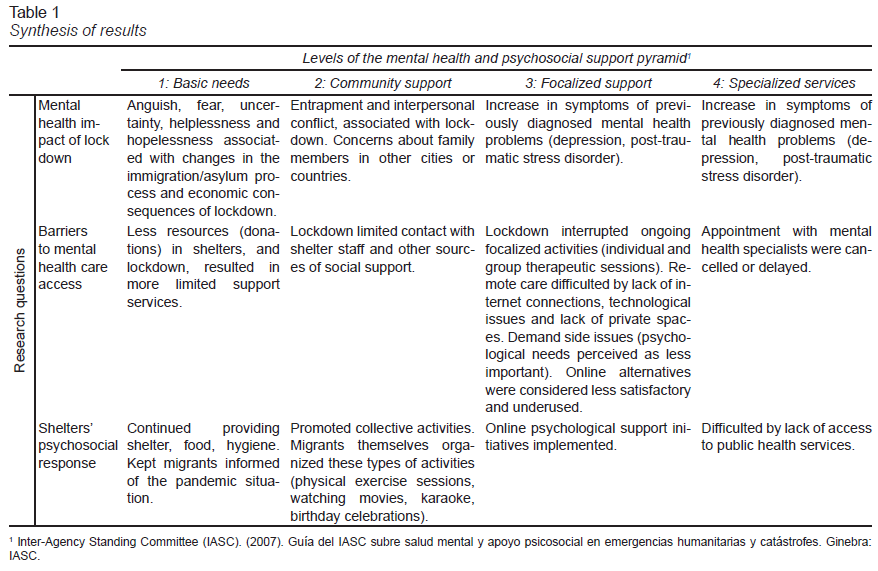
According to the usual practices for rapid qualitative studies (Taylor et al., 2018), in order to provide timely information about an ongoing situation we reduced data collection time, did not aim for data saturation, relayed on untranscribed interviews and notes, and summarized the results (instead of formal coding). Thus, we prepared a data analysis matrix (as reflected in Table 1) based on the four levels of the IASC pyramid. The pyramid for mental health and psychosocial support proposed by the United Nations’ Inter-Agency Standing Committee (IASC) (IASC, 2007) distinguishes four levels of support that humanitarian actors should aim to provide in order to protect mental health and psychosocial well-being in the midst of crisis: basic services and security (shelter, food, etc.), community and family support (facilitating access to social support, mobilizing existing social networks or creating new ones), focused-non specialized support (individual or group interventions to address psychological needs, including psychological first aid and basic mental health care), and specialized mental health services. For analysis, we combined the pyramid’s levels and the three main research questions (mental health impact of the lockdown, barriers to mental healthcare access, and psychosocial responses by the shelters), and situated participants’ responses in the cells thus defined. Analysis was conducted by all authors, and the conclusions discussed among them. Data related to mental health and access to mental healthcare, obtained through interviews and participant observation in the parent study, was employed to obtain a better understanding and validate the issues raised by participants in this rapid study.
Ethical considerations
The parent project was reviewed and approved by the Research Ethics Committee of El Colegio de la Frontera Norte (no. 058-032019). Interviewees gave verbal consent to participate in online or phone interviews, and were aware of the nature of the research project, risks and benefits, and of the voluntariness of their participation. Confidentiality of interviewees and shelters is preserved in the manuscript by not providing names or other identifiable details.
Results
Seven participants took part in the interviews. One of them works at two migrant shelters, so we were able to obtain information pertaining to a total of eight shelters. Participants’ age range is 25 to 55 years. All of them are Mexican, six females and one male. Two are mental health professional providing care at the shelters, one a social worker who is part of the shelter staff, and the other four have diverse responsibilities as part of the organization (director, coordinator, etc.)
In this section, we present the results regarding the impact of the pandemic and lockdown measures on migrants’ mental health, barriers to healthcare, and psychosocial support by the shelters. In each subsection, we go from a description of issues related to levels 1-2 of the IASC pyramid (psychological distress, basic needs and community issues) to those in levels 3-4 (problems requiring focalized and specialized care). The main results are summarized in Table 1.
Impact of the pandemic and lockdown on migrants’ mental health and psychosocial wellbeing
According to interviewees, the COVID-19 pandemic and lockdown measures impacted migrants’ mental health in ways that have been previously reported for the general population (Mukhtar, 2020), with anguish and fear related to concerns about the health risks and economic consequences. However, some aspects were specific to the migrants’ situation, among them increased uncertainty about their asylum application process, feelings of entrapment while sheltering in place, and the challenges of living in a non-private space.
As for the first aspect, many migrants in the shelters were at some step in their process of applying for asylum in the United States. At the time international border closures and lockdown measures defined by the shelters’ directives and Mexican authorities began, asylum applicants were either waiting to attend consecutive court hearings or to have their first-time interviews. At the time this research was conducted, the United States government had already twice moved all appointments to later dates. Migrants in this situation experienced increased uncertainty that translated into feelings of anxiety, low spirits (desánimo) and hopelessness. According to some interviewees, these feelings were already prevalent before, as part of a general attitude of “being on hold” (estar a la espera), in which migrants lived day to day, without knowing how long the wait would last or what the outcome of their asylum request would be. The pandemic was “one thing more on top,” increasing the distressful feelings for some, while for others it just seemed to be more of the same.
“... that’s what we’re doing here, waiting, but the truth is it hasn’t been easy because I have changes of mood, the hormones, everything exasperates me, I want to leave, to jump the [BORDER] wall” (Female Central-American asylum seeker, interviewed before pandemic).
Concerning the second aspect, increased feelings of entrapment were mentioned by most informants. According to them, younger migrants, and those who had jobs in the city, especially resented having to stay in the shelters during lockdown. Even if the shelters provided food and covered the basic needs of migrants, some still need money for themselves and their families (including those who usually sent remittances to families back in their country of origin), so being unable to work made them sad and frustrated. Beyond that, some migrants came from experiences of detention, or of being retained by kidnappers, so confinement was especially difficult for them.
“Right now, with the quarantine, you can see how they’re anxious at being locked-in. It’s like, I’m just coming from a prison in the US and now I’m locked-in again.” (Shelter social worker, during pandemic)
The third psychosocial aspect mentioned by interviewees was the difficulties of living in close quarters with strangers. As we will see below, migrants living in the shelters formed positive bonds and support networks, but there were also conflicts between them, and sometimes with the shelters’ personnel. These issues were also present before the lockdown, but surfaced in discussions about the decision to lockdown the shelters.
On the other hand, although we did not directly collect data on the prevalence of mental health problems, according to interviewees, previous manifestations of depression and anxiety also increased among those who already had them, and the symptoms of pre-existing disorders were exacerbated among some migrants who had previously been diagnosed with mental health issues. Interviewees reported that there were symptoms of post-traumatic stress disorder and anxiety among some who felt that the asylum process delay was forcing them to stay in a city where they did not feel secure, and also because of actual violence occurring close to some shelters during the period. As for substance use, most shelters do not receive people with substance use disorders, but some migrants who use tobacco, alcohol or drugs are able under normal circumstances to do so away from the shelters. This was impossible during lockdown, and according to one interviewee was the reason some migrants decided to leave the shelter. According to another informant, substance use increased among migrants living out of the shelters, as they worried about losing their jobs and the increased difficulties of obtaining asylum in the United States or regular migration status in Mexico. Those who decided to stay in shelters also had a difficult time in relation to their substance use.
“Right now, with the contingency, a person who is an alcoholic and a kid with addictions are a bit anguished. They told me they’re feeling very anguished [...] Up till now it’s OK, even while they’re in abstinence [BECAUSE OF THE LOCKDOWN], but they look fine...” (Shelter director, during pandemic)
Barriers to mental healthcare during the pandemic and lockdown
As is the case for other health problems (Leyva Flores, Infante Xibillé, & Quintino Pérez, 2016), mental health treatment for migrants is mainly provided by volunteers, CSOs and international agencies working in the shelters. The pandemic and lockdown impacted these services. The shelters received less material and financial donations with which to support their many activities, so they had to cut back in some. Physical distancing measures limited the visits of psychologists and other mental health care providers, interrupting individual and group therapies. For the same reason, as shelter staff continued working only from their own homes, the opportunity for daily casual contact between migrants and staff was lost. This type of contact had previously been a source of emotional support for migrants, an opportunity to vent emotional issues informally, whilst now those issues could only be discussed in the more structured environment of the continuing group sessions, or by special appointment, making communication more difficult for some.
At the time of interviewing, diverse organizations had activated online or over the phone free mental health care. However, according to interviewees these services were being underused by migrants in the shelters. The main reason they mentioned for migrants’ not using remote services was their lack of recognition of mental health problems as something requiring care, especially for issues perceived as minor such as depression or anxiety symptoms. The second was that in-person contact was important. A third barrier might have been that not all shelters had a private space where a migrant could go to call or connect to a therapist or counselor: only one interviewee mentioned that the shelter had such a place available, a measure they had taken since before the pandemic.
On the other hand, data from our ethnographic study reveals that barriers to specialized mental healthcare were apparent since before the pandemic. Besides the scarcity of public mental health services that affects the general population, migrants face other difficulties, among which are bureaucratic barriers, and waiting times of up to months before seeing a psychiatrist. During the pandemic, these barriers increased. According to informants, some migrants who were in treatment had to interrupt it because of the pandemic. Those who were already on medications were not able to buy them because of a lack of money due to job loss, while others who needed to renew their prescription were not able to do so, as appointments with psychiatrists were cancelled or waiting times made longer.
“Unfortunately, the migrant population always has problems to access health services, because they have no documents, they send them back [FROM THE UNITED STATES] without documents. Then, they have to go see the general practitioner first, then they’re referred to the psychiatrist, now is even more difficult” (Shelter social worker, during pandemic)
The psychosocial response of CSOs
According to our ethnographic study, migrant shelters are the main, and sometimes the only, providers of psychosocial support for migrants in levels 1 and 2 of the IASC pyramid in Tijuana. Having a roof over one’s head and food assured can make an enormous difference in mental health in dire situations (IASC, 2007), and by providing a safe place to stay and other services, such as legal counseling or help obtaining employment, the shelters support migrants in their basic needs. As for community support, the shelters help migrants to contact their families, organize language lessons and training programs, or offer religious services, all of which promotes the creation of new social networks and the activation of existing ones. Some shelters also have group activities intended for mental health promotion, such as arts and crafts groups or physical activities, and some run self-help groups or have access to psychologists who can provide family or individual care (level 3-4 of the IASC pyramid).
Most of these services were interrupted since the beginning of the lockdown, when the shelters limited the presence of volunteers and all but essential personnel in the premises in order to prevent contagion. However, some activities were subsequently adapted to continue online, and shelters with access to equipment such as projectors or wide screens had an advantage in this sense, while others were limited by their access to computers or Wi-Fi. In other cases, the only way for migrants to take part in online activities was through their own cellular phones, which meant that within the shelter there was unequal access to those activities.
Also, new activities were implemented. Some shelters gave daily COVID-19 updates to participants. The internet was useful as a source of exercise lessons and movies. Most importantly, the continuous support of the shelters to migrants’ basic needs made them a source of security, which no doubt had positive consequences on their mental health.
“It’s good for them to know that we have everything that they need to be well through this time” (Shelter director, during pandemic)
Besides the activities organized by the shelters, the migrants themselves suggested others, such as online delivered music therapy, art therapy and meditation. They also organized themselves to take zumba and dance lessons online. Other social activities organized by migrants included birthday parties for children and karaoke on weekends, all of which contributed to a sense of community within the shelters.
Discussion and conclusion
In this article, we have shown how the COVID-19 pandemic and lockdown measures had particular consequences on the mental health of migrants, and also affected their access to mental health care. The situation of migrants “stopped in motion” (Odgers-Ortiz & Olivas-Hernández, 2019) at the Mexico-United States border is akin to that of asylum seekers elsewhere, whose mental health is affected by lack of control over their future (Thomas et al., 2011) and uncertainty about their migration or asylum process (Haas, 2017; Niemi et al., 2019). While social isolation during lockdown can be a cause of mental health problems among the general population (Mukhtar, 2020), for migrants in shelters or camps overcrowding can also be an issue (Júnior et al., 2020). Those with pre-existing mental health problems such as depression or post-traumatic stress disorder could be particularly affected, as the lock down conditions replicate previous traumatic experiences and access to specialized care becomes even more difficult than usual.
All over the world, migrants face barriers to healthcare (Abubakar et al., 2018). In Mexico, migrant health policies have traditionally addressed the needs of Mexican migrants with minimal attention to the needs of in-transit migrants or asylum seekers (Bojorquez-Chapela, Flórez-García, Calderón-Villarreal, & Fernández-Niño, 2020). If access to mental health care is difficult for the general population (Berenzon Gorn, Saavedra Solano, Medina-Mora Icaza, Aparicio Basaurí, & Galván Reyes, 2013), it is even more so for migrants. This situation puts migrants in a particularly harsh situation during crisis such as the COVID-19 pandemic.
In the face of the above, the response of many CSOs operating migrant shelters in Tijuana was noticeable for its comprehensiveness. Building on an already existing network of volunteers and organizations, they adapted and implemented activities that conform to international recommendations for the psychosocial support of migrants and displaced populations in emergencies (IASC, 2007; International Organization for Migration [IOM], 2019). The importance of participating in activities with other migrants and refugees for social network strengthening and mental health has been repeatedly documented (Bulik & Colucci, 2019; Niemi et al., 2019; Thomas et al., 2011). At the same time, psychosocial support was limited by a lack of resources, including limited governmental support, as has been the case in other countries (Júnior et al., 2020). An issue worth noting (and studying in the future) was the way the migrants also responded by proposing and organizing diverse activities that helped to foster a sense of community between themselves. Resilience and agency are essential aspects of migrants’ and refugees’ experience that need to be considered when planning mental health actions in order to provide the conditions in which these characteristics can flourish (Tippens, 2017).
As compared to other qualitative methods, that typically involve a prolonged immersion in the field and an iterative process of analysis that also can take very long, rapid assessment methods are limited in the depth of information they provide. Another limitation of rapid qualitative studies is that they do not continue till theoretical saturation (the moment in a qualitative study when further data collection leads to the same conclusions already established) is reached. Our study was also limited in its scope, using data from a limited number of interviews conducted over a very short period. To address these limitations, we employed data from our ongoing ethnographic study, but findings might still be biased towards the view points of the selected informants. A major limitation is that the mental health consequences of the pandemic and lockdown were not ascertained from the migrants themselves. Also, migrants who remained in the shelters after lockdown might have been different from those who chose to leave, and according to at least one informant, the latter might be more at risk of substance-use related mental health issues.
Further research is needed to address these limitations, exploring the mental health consequences of the pandemic through interviews with a representative sample of migrants. The effectiveness of psychosocial interventions in this context also needs to be researched further with both qualitative and quantitative methods. Finally, the use of qualitative methods in the research of epidemics is in itself an important area of study (Teti, Schatz, & Liebenberg, 2020). All of these will be needed in order to obtain a more precise vision of the impact of a pandemic on the mental health of members of mixed migrant flows to validate our findings and to assess to what degree they are generalizable.
To conclude, our results suggest that, as other authors anticipated, the COVID-19 pandemic and lockdown measures have important mental health consequences for migrants. Pandemic preparedness plans thus far have seldom considered the special needs of this group (Wickramage et al., 2018), and mitigation and containment measures can have serious, unintended consequences for this population ([IOM] Migration Health Division - Research and Epidemiology Unit, 2020). Members of mixed migration flows in Mexico require a tailored response to their mental health needs in the COVID-19 pandemic, as has been suggested for other socially excluded groups (Holmes et al., 2020). As recommended by international organizations, instead of being limited to clinical interventions, this response should prioritize the psychosocial aspects that are the root of mental health problems in these type of populations, covering basic needs such as decent work, appropriate places to live, and access to education and health services (IASC, 2007; Organización Internacional para las Migraciones (OIM), 2018). Migrant shelters constitute spaces where CSO’s, along with the migrant population, can creatively develop different strategies to tackle the hardships faced by migrants during the lockdown. The support of governmental and other agencies and coordination between the public health system and these organizations can make the response more efficient.