BACKGROUND
According to the fifth version of the Diagnostic Statistical Manual (DSM-V) of Mental Health, Post-Traumatic Stress Disorder (PTSD) is defined by symptoms related to five dimensions: Re-experiencing distressing events, hyperarousal (irritability, recklessness, hypervigilance, exaggerated startle response, concentration difficulties, and sleep disturbance), persistent avoidance, negative cognitions, and mood alterations, although complex symptoms include dissociation (American Psychiatric Association [APA], 2013). Dissociative symptoms can be manifested through depersonalization or feeling detached from one’s mental processes and derealization or experiencing unreality of surroundings (APA, 2013). All symptoms must be present after one month of experiencing an actual or threatened death, whether direct, witnessed, or learned (APA, 2013).
The National Institute for Health and Care Excellence (NICE, 2016a) suggests that suitable psychological treatment interventions in cases of PTSD are Trauma-focused Cognitive Behavioural Therapy (TF-CBT) and Eye Movement Desensitisation and Reprocessing (EMDR) in children and young people (CYP). In adults, the NICE (2016a) guidelines recommend Cognitive Processing Therapy, Cognitive Therapy (CT) for PTSD, narrative exposure therapy, prolonged exposure therapy, EMDR, and computerized TF-CBT if no severe symptoms or risk of harm are present. Interventions in adults and CYP are based on standardized manuals that aim to restructure the traumatic meaning and overcome avoidance, where follow-ups on dates significant to the event are considered (NICE, 2016a). In terms of differences, the NICE (2016a) guidelines emphasize that CYP interventions need to be adapted to developmental age and involve their respective caregivers whilst in adults the focus is on re-establishing adaptive functioning. Overall, the interventions recommended across the life span are individual in nature, and CT or Cognitive Behavioural Therapy (CBT) is referred to as evidence-based treatment.
As developed by Beck (1976/1989), CBT is an evidence-based model of psychological therapy built on the assumption that cognitions, emotions, behaviors, and physical sensations are interlinked in the creation of a vicious cycle that perpetuates the main problem. Because each of these four factors influences each other, if one of them were to be intervened, the others would most likely change in their presentation (Wills & Sanders, 2013). Whilst CBT aims to intervene in thoughts and behaviors, CT focuses purely on the cognitions involved under the premise that the event’s interpretation generates an emotion instead of the event by itself causing a particular emotion (Kennerley, Kirk, & Westbrook, 2007).
Regarding mindfulness, the NICE (2016b) guidelines maintain that Mindfulness-Based Cognitive Therapy (MBCT) is an evidence-based (EB) intervention that prevents relapse in depression or residual symptoms of depression, where low mood, anhedonia, and reduced energy levels are core symptoms. Thus, common domains affected between depression and PTSD are negative cognitions and mood alterations. Mindfulness, a Buddhist cultural tradition of meditation, has been broadly described as the ability to be purposefully attentive in the present moment, thus MBCT promotes self-awareness to generate a cognitive shift when negative mood alterations are experienced since they are not indicative of the present moment (Segal, Williams, & Teasdale, 2013). MBCT is inspired by the initial adaptation of mindfulness into a structured program for Western medical settings aiming to treat chronic pain, named Mindfulness-Based Stress Reduction (MBSR), an eight-week group intervention focused on promoting awareness of thoughts and physiological responses through meditation, breathing exercises, and yoga (Kabat-Zinn, 1994). Although the NICE (2016c) guidelines do not recommend MBSR for the treatment of mental health conditions, it is acknowledged that significant improvements have been found in the treatment of social anxiety disorder (Norton, Abbott, Norberg, & Hunt, 2015).
The rationale of this review
Acknowledging the role of MBCT or MBSR in the treatment of PTSD can inform clinicians’ practice and prevent iatrogenic effects on clients. The NICE (2016a) guidelines recommend standardized interventions applied by trained practitioners with ongoing supervision in cases of PTSD. Therefore, mindfulness-based interventions have only recently been considered a treatment of choice since a valid manual for MBSR and MBCT was not available until 1990 (Kabat-Zinn, 1994) and 2002 (Segal, Williams, & Teasdale, 2013) respectively. Since one teacher can conduct these group interventions remotely, their implementation might have a positive impact whilst coping with the COVID-19 pandemic through public health measures, such as isolation (World Health Organization, 2020). Thus, the current review will provide evidence of affordable interventions, which in addition to minimising treatment waiting time for mental health services, create the potential to prevent relapse in clients after completion of treatment (NICE, 2016b).
Previous reviews
Because MBSR and MBCT are treatments based on a valid manual, previous reviews have focused their attention on these two types of mindfulness-based interventions solely. Authors concluded that whilst MBSR reduces PTSD symptoms through fear extinction (Kummar, 2018), MBCT restructures traumatic memories, although further research is needed by adding neuroimaging techniques, non-veteran populations, and comparing its effects to other therapeutic interventions (Williston, Grossman, Mori, & Niles, 2021). Nevertheless, new articles have been published since the above previous reviews. Therefore, additional information must be addressed in terms of filling the current gaps in the literature.
Objectives
The present review of scientific journals aims to systematically review and update existing literature about the association between PTSD and MBCT or MBSR. The objectives have been listed as follows.
To review existing literature about the association between standardized mindfulness-based interventions and PTSD. Particularly, the current study aimed to provide a critical appraisal of the published literature in terms of research methodology.
To identify implications for practice and recommendations for future research. Particularly, the current study aimed to provide a critical appraisal of the published literature in terms of populations, outcome measurements, and intervention formats that have been examined.
METHOD
Databases and search
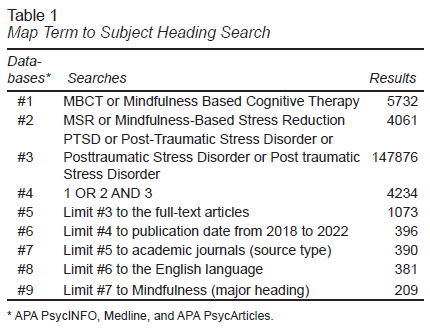
The CINAHL Complete, PsycINFO, Medline, and PsycArticles databases were searched to select studies for inclusion in this review. Search keywords used were MBCT or Mindfulness-Based Cognitive Therapy OR Mindfulness-Based Stress Reduction or MBSR AND Post-Traumatic Stress Disorder or PTSD, looking for full-text articles from 2018 up to march 2022. Details of the databases and search strategy are provided in Table 1.
Inclusion criteria
Publications were included independent of the population’s age, gender, intervention format, and the methodology used.
Articles involving active military service members or war veterans were included due to the representativeness of the sample.
Exclusion criteria
Publications referring to trauma or posttraumatic stress (PTS) instead of referring to PTSD were excluded.
Articles not referring to MBCT or MBSR were excluded.
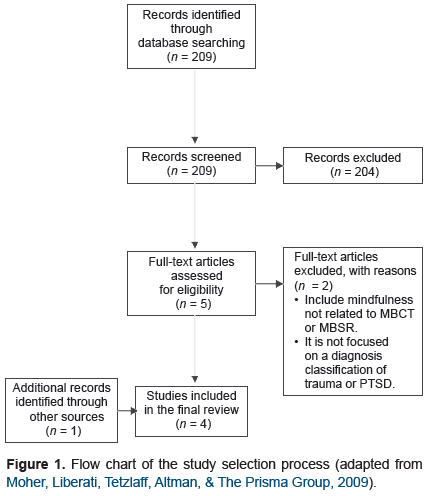
Data extraction and screening process
209 articles were identified through the search and filter of electronic databases, where a two-step screening process was applied. 204 were excluded based on the title. Of the remaining five articles, two were excluded following a review of the abstract and full article against the exclusion criteria as detailed above. Consequently, previous reviews were examined to fill in the gaps of already published work and for any studies that were missed in the database searches. Therefore, a total of four papers were selected for the purposes of this literature review. Figure 1 shows a flow chart of the study selection process.
RESULTS
Quality assessment
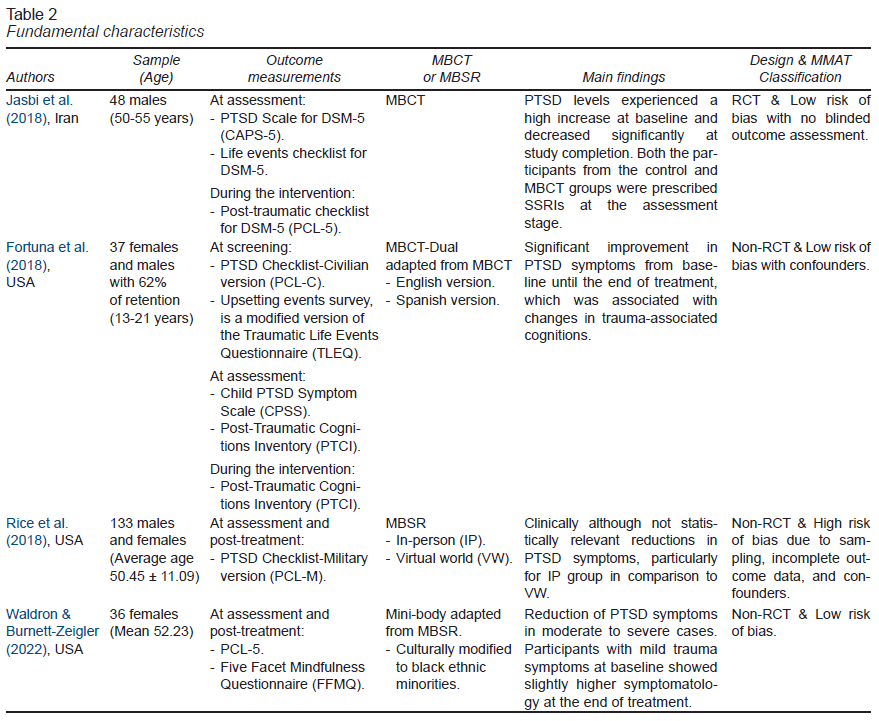
After full-text evaluation, the risk of bias was assessed using the assessment method MMAT (Hong et al., 2018). Key quality criteria under evaluation for the quantitative randomized controlled trials (RCT) were appropriate balance and allocation to intervention or control group, completion of outcome data, blinded outcome assessment, and dropout rate. For the other three quantitative non-randomized controlled trials, sample representativeness, completion of outcome data, confounders accountability, and adherence to the planned intervention were considered. The studies were then classified as low if up to a maximum of one criterion had not been accomplished, or high for risk of biases. For a detailed overview of the quality assessment (Table 2), which provides a summary of its fundamental characteristics.
In what populations has the effectiveness of MBCT and MBSR been tested?
Three of these studies were conducted on adults with exception of Fortuna, Porche, and Padilla (2018), where the participants were adolescents. The population presenting PTSD were military active service members, war veterans, adolescents, and black women. Respectively, the rationale to include these populations is that current, or past involvement in acts of war is considered a life-threatening event. Adolescents were included in Fortuna et al. (2018) research because they had experienced a variety of traumatic events one or more times, such as assault, physical or psychological abuse, loss, or serious injury in an accident. Black women were recruited on the basis that female gender due to genetic vulnerability, ethnic minority background, and socioeconomic disadvantage are risk factors for traumatic experiences (Waldron & Burnett-Zeigler, 2022). The participants had survived one to nine different types of traumas, where physical and sexual abuse were the most common.
What formats of MBCT and MBSR have been offered?
Although the format of the intervention varied alongside the four items of research, all of them included face-to-face sessions, an 8-week intervention, and did not have a follow-up after the end of the treatment. Exceptions were Fortuna et al. (2018), which aimed for a 12-week intervention, and Rice, Liu, and Schroeder (2018), which included virtual sessions. The format of each research is described in the following lines.
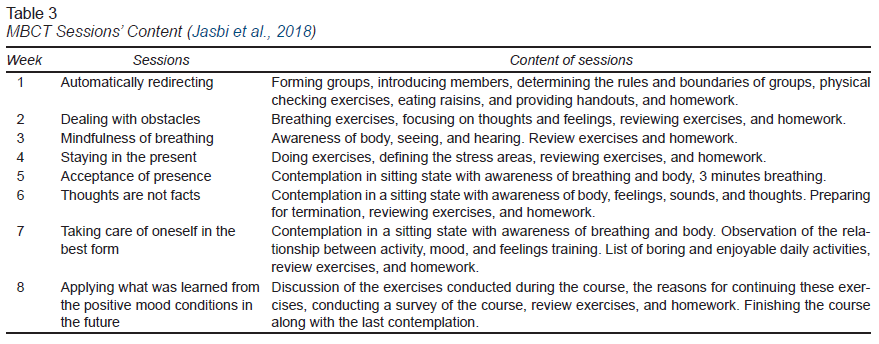
Jasbi et al. (2018) delivered MBCT in a group format of 8-week, where each weekly session lasted between 60 to 70 minutes and the group size varied from 7 to 12 participants. The content of the MBCT sessions is detailed in Table 3.
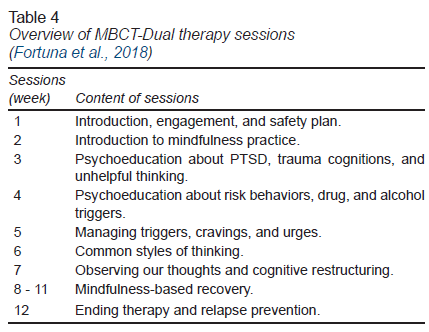
Fortuna et al. (2018) used a TF-CBT adaptation for adolescents known as MBCT Dual, combining MBCT with relaxation and breathing retraining (Rosenberg, Jankowski, Fortuna, Rosenberg, & Mueser, 2011). The intervention is conducted in a group format intended to last for 12 weeks although the study only had a 6-week retention. Weekly therapy sessions were 50 to 60 minutes in length. It is worth mentioning that the intervention was delivered in Spanish to 11 of the participants, who were primarily Spanish monolinguals. An overview of MBCT-Dual therapy sessions is provided in Table 4.
Rice et al. (2018) considered weekly in-person (IP) and virtual world (VW) MBSR in different groups of eight weeks each, where VW training involved avatar-to-avatar interaction. The IP group met between two and 2½ hours with an “all-day” silent class of 3½ hours whilst the VW group met for 1½ hours per week with a silent class under the same conditions as the IP group.
Waldron & Burnett-Zeigler (2022) carried out an mind-body intervention adapted from MBSR that focuses on cultivating non-judgmental awareness of the body, maintaining the length of the intervention and content of the sessions (meditation, yoga, body scan, and social interaction). However, the length of the sessions was 90 instead of 180 minutes, which were conducted by a trained health educator, and the program materials related to black artists to reflect the participants’ experiences.
What outcome measurements have been used to monitor PTSD symptoms and mindfulness?
With regards to PTSD outcome measures, all studies used the post-traumatic checklist for DSM-5 (PCL-5) or its variations, although the methodology varied with regards to the application of this measurement, with only two applying the questionnaire at the assessment and post-treatment stage (Rice et al., 2018; Waldron & Burnett-Zeigler, 2022). The PCL-5 consists of a 20-item self-assessment questionnaire of symptoms related to the five dimensions identified in PTSD, where answers are given on five-point Likert scales ranging from 0 (not at all) to 4 (extremely; Blevins, Weathers, Davis, Witte, & Domino, 2015). Expanding on its variations, Fortuna et al. (2018) applied the PTSD Checklist-Civilian version (PCL-C), a 17-item version of the PCL recommended for civilian populations where multiple traumas are present (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). Rice et al. (2018) used the PTSD Checklist-Military version (PCL-M), a 17-item self-report focused on stressful military experiences (Blanchard et al., 1996).
In relation to mindfulness, only one of the studies aimed to monitor changes in awareness. Waldron and Burnett-Zeigler (2022) utilized the Five Facet Mindfulness Questionnaire (FFMQ), which is a 39-item self-report questionnaire of 5 domains identified in mindfulness: Describing, acting with awareness, non-judging, non-reacting, and observing (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006).
What are the results of MBCT and MBSR interventions in the treatment of PTSD?
Regarding MBCT, Jasbi et al. (2018) found that PTSD levels experienced a high increase at baseline in the intervention group and then decreased significantly over time in comparison to the control group. Similarly, in Fortuna et al. (2018) research, there was a significant improvement in PTSD symptoms from baseline until the end of treatment, which was associated with changes in trauma-associated cognitions. There was also a significant reduction in the frequency of substance misuse.
Concerning MBSR, Rice et al. (2018) found that IP and VW are both effective in the reduction of PTSD symptoms in comparison to the control group, although the IP group showed a greater reduction in PTSD symptoms. Along the same lines, the results of Waldron and Burnett-Zeigler (2022) suggest a significant reduction of PTSD symptoms from baseline to end of treatment and an increase in Mindfulness measured by the FFMQ. Nevertheless, a minority of participants that exhibited mild trauma symptoms at baseline, showed slightly higher symptomatology at the end of treatment. The researchers assumed that these women may have been retraumatized by becoming more aware of their thoughts, emotions, and physical sensations without an intervention aiming to change their experience. Conversely, the results also found a correlation between session attendance and PTSD symptom remission, where women with a higher PTSD symptomatology attended more mindfulness sessions. Finally, there were no statistically significant differences in the results between different trauma types.
DISCUSSION AND CONCLUSION
Critical appraisal of the association between MBCT or MBSR and PTSD
Overall, the four pieces of research do not provide extensive details to determine the active components of MBCT or MBSR which have an impact on symptoms reduction. The change in PTSD symptoms in terms of questionnaire items or thinking processes is not reported in the results. Furthermore, the change in underlying mechanisms attached to the practice of mindfulness is only monitored in one of the articles through the FFMQ.
In terms of research methodology, none of the papers included a follow-up to monitor if the improvement in PTSD symptomatology had been maintained over time. Only two of the four studies had a control group with only Jasbi et al. (2018) being an RCT with a low risk of biases. Whilst in Jasbi et al. (2018), the control group was offered socio-therapeutic events (short trips or medical checks), Rice et al. (2018) maintained the control group on a waiting list and invited the participants to MBSR groups after the trial had ended. Hence, the latter does not control for non-therapeutic factors, such as social support and the effect of receiving professional help.
Subsequently, the MMAT classification (Hong et al., 2018) suggests that the research by Rice et al. (2018) presents a high risk of biases due to the presence of confounders and in terms of sample representativeness. In comparison to other studies, a clear description of the participants is not included, where military service populations were invited after completing the PCL-M without specifying if PTSD criteria had been met or if their initial symptoms were over the threshold. Furthermore, nine of the PCL-M results were not included due to computer error, which accounts for incomplete outcome data.
Focusing on the acknowledgment of confounders among the four articles, only two addressed comorbidities among the samples presenting significant PTSD symptoms. Particularly, attentional deficit and hyperactivity (ADHD) in Rice et al. (2018) and Fortuna et al. (2018), where the adolescent population also presented substance misuse. Because the DSM-V (2013) characterized ADHD as difficulties with inattention among other criteria, Rice et al. (2018) did not control for ADHD on the basis that similar symptoms can be caused by PTSD’s hyperarousal. Similarly, Fortuna et al. (2018) attributed substance misuse to the PTSD diagnosis with cannabis, alcohol, or methamphetamines offering a short-term relief for survivors. Consequently, medication as an additional intervention is found in Jasbi et al. (2018) and Fortuna et al. (2018). The first considered MBCT as an adjuvant to Selective serotonin reuptake inhibitors (SSRIs) and the second included adolescents under the prescription of SSRIs, bupropion, or methylphenidate if the participants were on a stable dose for the previous 8 weeks. After mentioning that methylphenidate had been prescribed to a percentage of the adolescents, Fortuna et al. (2018) mentioned that some of the participants were diagnosed with ADHD, which is not previously recognized in the sample description nor controlled for.
With regards to the intervention’s format, three of the studies aimed to improve retention rates by providing MBSR adaptations. Firstly, Rice et al. (2018) delivered a virtual format of MBSR, where the participants could remain anonymous. Secondly, Waldron and Burnett-Zeigler (2022) provided a culturally adapted MBSR hosted in a community setting by a representative member of the sample. Thirdly, Fortuna et al. (2018) provided the opportunity to work with matched Spanish-speaking providers. Even though these interventions promoted adherence to the treatment, limitations are also recognized. The former, due to its virtual nature where the participants interacted through an avatar with other members of the group, made it impossible to control for participant’s involvement. On a different turn, Waldron and Burnett-Zeigler’s (2022) results have implications in terms of replication, considering that mini-body sessions’ content is not outlined, nor is the training conducted by the facilitator. A similar gap in terms of the facilitator’s expertise is found in Jasbi et al. (2018), with CBT therapists and MBSR instructors carrying out a different modality of mindfulness, MBCT.
Despite the previous points for improvement, the uniqueness of the research papers is one of its strengths since these appear to be the first attempts to investigate whether a standardized mindfulness-based intervention is a suitable intervention for PTSD clients presenting different types of severity. Therefore, the articles could be considered a first step toward informing further research on the topic. From the results, MBCT and MBSR seem to tackle different domains of the diagnosis, whereas Rice et al. (2018) emphasize the improvement in terms of attentional difficulties with whether IP or VW MBSR, which corresponds to the PTSD domain of hyperarousal. Meanwhile, Jasbi et al. (2018) mentioned that by the fourth and fifth sessions, participants were listing their dysfunctional cognitive concepts and linking them to the avoidant behaviors maintaining their symptomatology. Comparing both interventions, the studies suggest that an increase in symptomatology is expected when clients are due to commence the treatment. An eventual decrease in PTSD symptoms is expected for MBCT participants with mild, moderate, and severe presentations whilst MBSR was proven effective only for the latter two.
Implications for practice
MBCT, MBSR, and its adaptations have been safely tested with active military service members, war veterans, ethnic minorities, and adolescents who have been affected by different types of traumas. MBCT-Dual and mini-body are adaptations from MBCT and MBSR, where relaxation and breathing retraining or non-judgmental awareness of the body are attempted, respectively. In addition, virtual reality and culturally informed formats have been delivered to reduce the stigma associated with mental health, where attention to the session’s content, facilitator’s background, and language had a positive impact on retention rates. All the studies used the PCL-5 or its variations to monitor PTSD symptoms, with one using the FFMQ to monitor changes in awareness.
Despite its limitations, the findings add to our understanding of the complexities of treating PTSD in different populations. In these contexts, there is moderate evidence to support the notion that MBCT, MBSR, or its adaptations are effective in reducing PTSD symptomatology. Empirically, the role of MBCT has been proven in the reduction of cognitive alterations and comorbid substance misuse. Nevertheless, caution should be taken at baseline, where clients could experience an increase in their symptoms. On the other hand, MBSR tackled the hyperarousal of clients who experienced moderate to severe symptoms, whilst being iatrogenic for baseline mild trauma symptoms which had increased at the end of treatment. Although the higher symptomatology rates at the end of MBSR could be due to the higher attendance of participants presenting moderate to severe PTSD symptoms, a sensible practice would be only to conduct MBSR under these conditions.
Recommendations for future research
Methodologically, future studies will be enhanced by testing MBCT, MBSR, and its adaptations in a particular type of trauma and tailoring the intervention to a specific cultural background. Participants from both genders could be included although separated groups might be needed due to the nature of the trauma. A randomized controlled design, controlling for social interaction and professional care in the control group can aid the comparison with the intervention group. Due to the complexity of the disorder, comorbidities must be acknowledged and managed to inform the findings, such as secondary diagnosis and adjuvant interventions. While MBCT has been added to pharmacological treatment, it is unknown if it could be an adjuvant to other psychological interventions suggested by the NICE Guidelines. Including trained instructors at an expert level in each treatment modality might have an impact on producing statistically significant results. Because MBSR and MBCT have an impact on different domains of the disorder, reports need to cover exhaustively the content of the sessions, where the incorporation of neuroimaging techniques can be valuable in symptoms monitoring. Formats where the participants do not remain anonymous and engagement can be controlled aid more information to the results, where the effectiveness of online treatment is still to be investigated. To conclude, the inclusion of a follow-up is relevant in determining if the improvements can be maintained without the support of a qualified practitioner.
Registration and protocol
The review was not registered. The protocol was prepared and amended as part of the CBT Postgraduate Diploma at Coventry University.