Regístrate en 1Win Colombia y Aprovecha los Mejores Bonos de Bienvenida

¿Qué es 1Win y por qué es popular en Colombia?
1Win es una plataforma internacional que ofrece servicios de casino online y apuestas deportivas. Desde su lanzamiento, ha capturado la atención de muchos usuarios en Colombia, gracias a su variada oferta de juegos, atractivas bonificaciones y la facilidad de acceso a través de su sitio oficial de 1Win.
La popularidad de 1Win Colombia se basa en varios factores clave:
- 1. Variedad de Juegos y Apuestas: La plataforma cuenta con una extensa selección de juegos de casino, incluyendo tragamonedas, ruleta, póker, y una sólida oferta de apuestas deportivas que cubre eventos locales e internacionales.
- 2. Bonificaciones y Promociones: 1Win es conocido por sus generosos bonos de bienvenida y promociones continuas, lo que atrae tanto a nuevos usuarios como a jugadores experimentados.
- 3. Accesibilidad: La plataforma es fácil de usar y está disponible en múltiples dispositivos, permitiendo a los usuarios colombianos acceder desde cualquier lugar y en cualquier momento.
- 4. Seguridad y Confiabilidad: Aunque opera bajo una licencia internacional, 1Win Colombia se compromete a proporcionar un entorno seguro para sus usuarios, garantizando la protección de sus datos y transacciones.
- 5. Soporte al Cliente: 1Win ofrece un servicio de atención al cliente eficiente, disponible 24/7 para resolver cualquier duda o problema que puedan tener los usuarios.
- 6. Métodos de Pago Diversificados: Los usuarios pueden elegir entre una amplia gama de métodos de pago, incluidos tarjetas bancarias, monederos electrónicos, y criptomonedas.
A continuación, se presenta una tabla con información clave sobre 1Win Colombia:
Cómo Registrarse en 1Win Colombia: Guía Paso a Paso
Registrarse en 1Win Colombia es un proceso sencillo que permite a los nuevos usuarios acceder a una amplia variedad de juegos de casino y opciones de apuestas deportivas. A continuación, te ofrecemos una guía paso a paso para completar tu registro en 1Win y empezar a disfrutar de todos los beneficios que la plataforma ofrece.
Paso 1: Acceder al Sitio Oficial de 1Win
El primer paso para registrarte en 1Win Colombia es visitar el sitio oficial de 1Win. Puedes hacerlo desde cualquier navegador en tu PC o dispositivo móvil. Asegúrate de estar en la página correcta verificando que la URL empiece con "https://" para garantizar una conexión segura.
Paso 2: Iniciar el Proceso de Registro
Una vez en el sitio oficial de 1Win, busca el botón de "Registrarse" o "Sign Up", generalmente ubicado en la esquina superior derecha de la página. Haz clic en este botón para iniciar el proceso de creación de tu cuenta.
Paso 3: Completar el Formulario de Registro
Al hacer clic en "Registrarse", se abrirá un formulario que debes completar con tu información personal. Asegúrate de ingresar datos precisos y válidos, ya que esto es crucial para la verificación de tu cuenta. Los campos típicos que deberás llenar incluyen:
- Nombre completo: Tu nombre tal como aparece en tus documentos oficiales.
- Correo electrónico o número de teléfono: Un contacto válido donde recibirás confirmaciones y actualizaciones.
- Contraseña: Crea una contraseña segura que contenga letras, números y símbolos para proteger tu cuenta.
Paso 4: Seleccionar la Moneda y Aceptar los Términos
En este paso, tendrás que seleccionar la moneda que prefieres utilizar en tu cuenta. Es importante hacer esta elección cuidadosamente, ya que cambiar la moneda después del registro puede ser complicado. Además, deberás leer y aceptar los términos y condiciones de uso de la plataforma antes de continuar.
Paso 5: Confirmar el Registro
Una vez que hayas completado todos los campos, haz clic en "Registrarse" o "Crear Cuenta". En este punto, es posible que recibas un correo electrónico o un mensaje de texto con un enlace o código de verificación. Asegúrate de seguir las instrucciones para confirmar tu cuenta y activar el acceso completo a la plataforma.
Paso 6: Hacer el Primer Depósito y Reclamar el Bono de Bienvenida
Después de completar tu registro en 1Win, puedes iniciar sesión y realizar tu primer depósito. 1Win Colombia ofrece un bono de bienvenida para nuevos usuarios, que puedes reclamar al hacer tu primer depósito. Este bono puede aumentar significativamente tu capital inicial para apuestas y juegos en el casino.
1Win Instalar
Instalar 1Win en tu dispositivo es un proceso sencillo. Para instalar 1Win en Android, descarga el archivo APK desde el sitio oficial, habilita la instalación desde fuentes desconocidas en tu dispositivo, y sigue las instrucciones. Para iPhone, simplemente busca 1Win en la App Store e instala la aplicación como lo harías con cualquier otra.
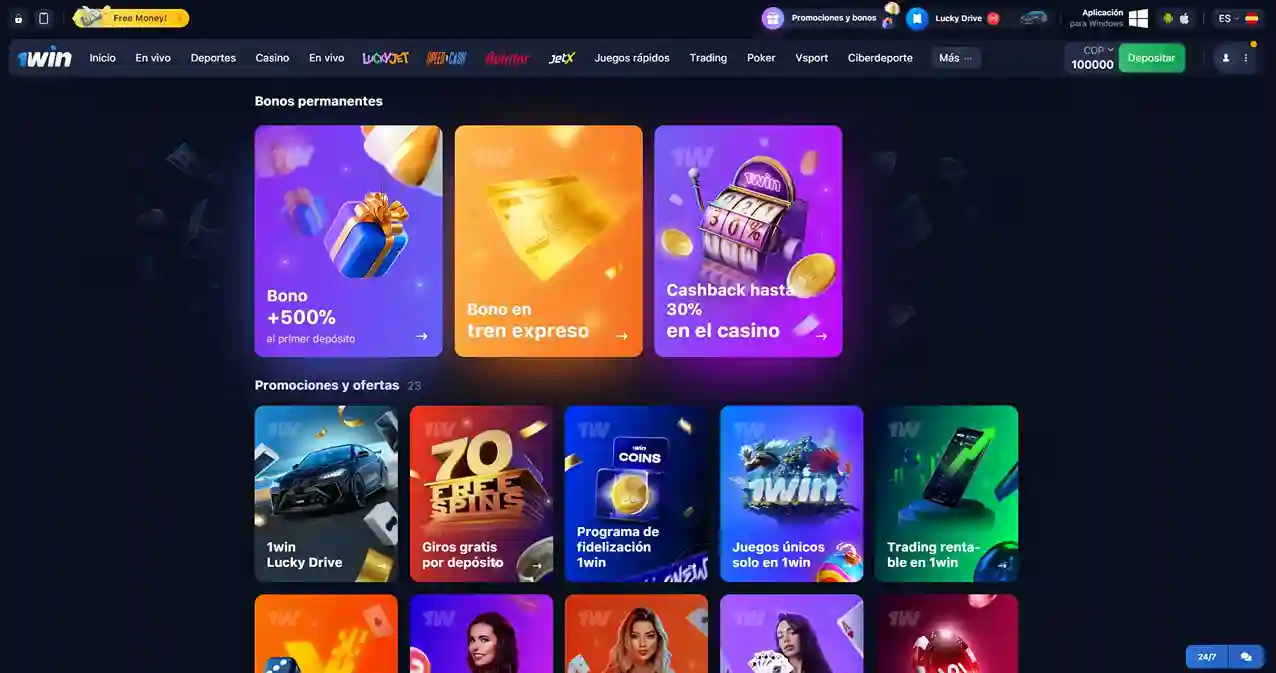
Bono de Bienvenida de 500% en 1Win: Cómo Funciona
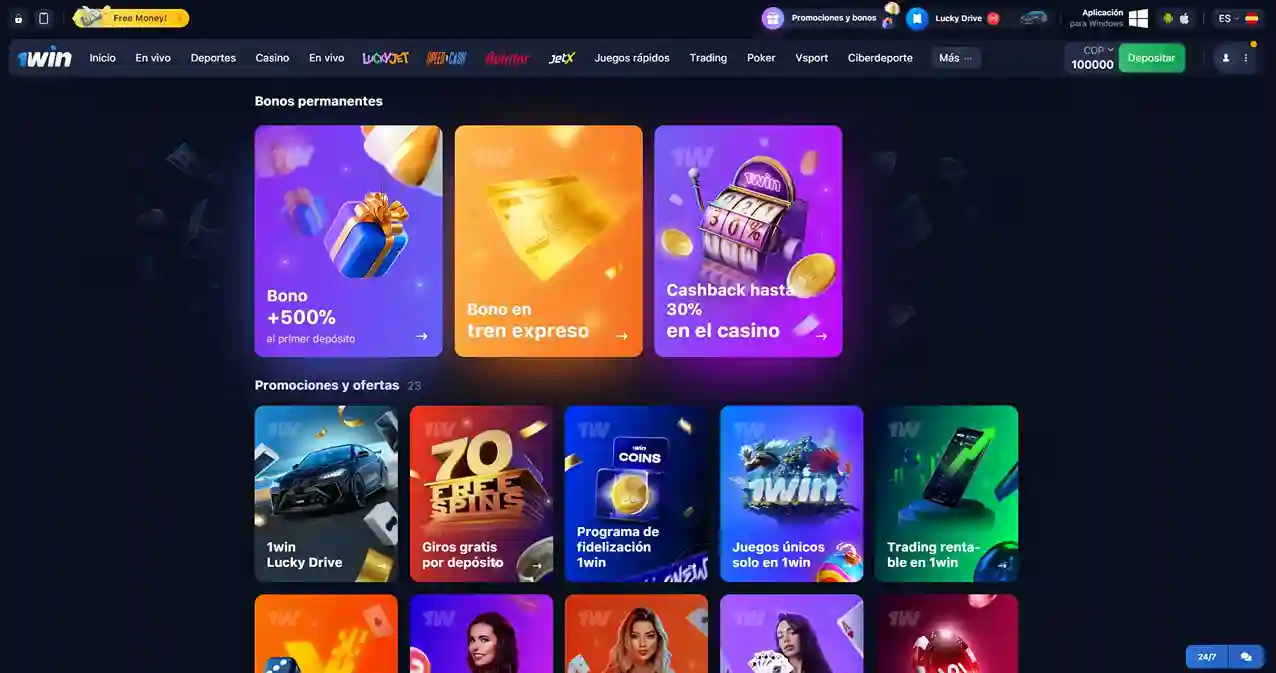
Uno de los mayores atractivos de 1Win es su generoso bono de bienvenida, que ofrece a los nuevos usuarios la oportunidad de aumentar significativamente su capital inicial. Este 1Win bono es una excelente manera de comenzar en la plataforma, ya que permite a los jugadores explorar más juegos y realizar apuestas con un mayor fondo. A continuación, te explicamos en detalle cómo funciona este bono 1Win y cómo puedes aprovecharlo al máximo.
¿Qué es el Bono de Bienvenida de 500% en 1Win?
El bono de bienvenida de 500% en 1Win es una oferta exclusiva para nuevos usuarios que realizan sus primeros depósitos en la plataforma. Este 1Win bonus se aplica a los primeros cuatro depósitos que realices después de registrarte, lo que significa que puedes recibir hasta 500% de tu depósito inicial como saldo adicional en tu cuenta.
Cómo Funciona el Bono de Bienvenida
El funcionamiento del bono 1Win es bastante simple y se estructura de la siguiente manera:
En total, puedes obtener hasta un 500% de bono en tus primeros cuatro depósitos, lo que representa una excelente oportunidad para maximizar tus fondos y explorar todo lo que 1Win tiene para ofrecer.
¿Cómo Obtener el Bono?
Para recibir este 1Win bono, simplemente sigue estos pasos:
- 1. Regístrate en 1Win si aún no lo has hecho. Puedes seguir las instrucciones del proceso de registro para crear tu cuenta.
- 2. Realiza tu primer depósito en la plataforma. Asegúrate de verificar la cantidad mínima requerida para activar el bono.
- 3. El bono se acreditará automáticamente en tu cuenta después de cada depósito. No es necesario que ingreses ningún código promocional, ya que el bono se aplica de manera automática.
Condiciones de Uso del Bono
Como con cualquier bonus, es importante leer y entender los términos y condiciones que lo acompañan. Algunos de los puntos clave incluyen:
- Requisitos de Apuesta: El bono debe ser apostado un cierto número de veces antes de que los fondos puedan ser retirados. Por ejemplo, es posible que necesites apostar el monto del bono 10 veces en apuestas con cuotas específicas.
- Cuotas Mínimas: Para cumplir con los requisitos de apuesta, las apuestas deben realizarse en eventos con cuotas mínimas establecidas, generalmente alrededor de 1.5 o superiores.
- Plazo de Validez: El bono tiene un plazo de validez limitado, generalmente dentro de los 30 días posteriores a su activación. Si no cumples con los requisitos dentro de este período, podrías perder el bono.
Maximiza el Uso del Bono
Para aprovechar al máximo el bono 1Win, aquí hay algunos consejos:
- Planifica tus Depósitos: Realiza depósitos estratégicos que te permitan maximizar el bono disponible.
- Juega Inteligentemente: Usa el bono en juegos o apuestas donde tengas una mayor probabilidad de ganar, y asegúrate de cumplir con los requisitos de apuesta.
- Mantente Informado: Revisa regularmente las promociones y ofertas en 1Win para asegurarte de no perderte otras oportunidades de bonificación.
El 1Win bonus de bienvenida es una oportunidad única para multiplicar tus fondos y explorar la plataforma con un mayor capital. Siguiendo los pasos y consejos anteriores, podrás sacar el máximo provecho de esta oferta y disfrutar de todo lo que 1Win tiene para ofrecer.
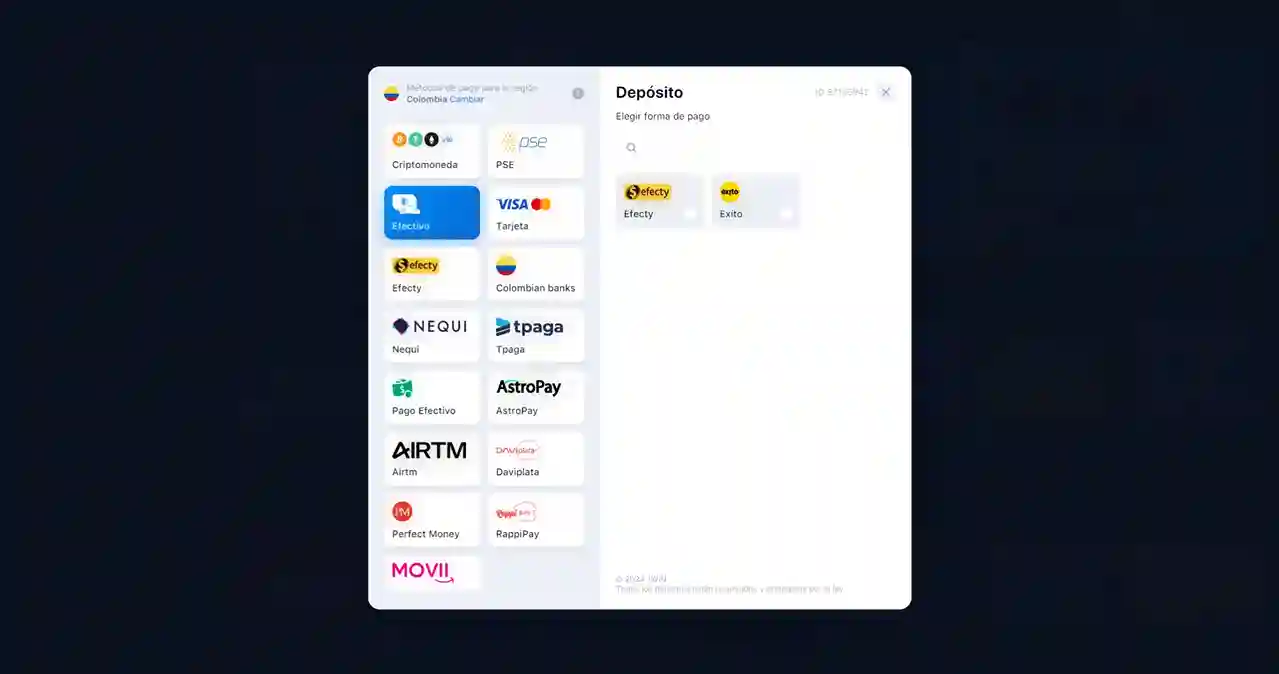
Métodos de Pago Disponibles en 1Win Colombia
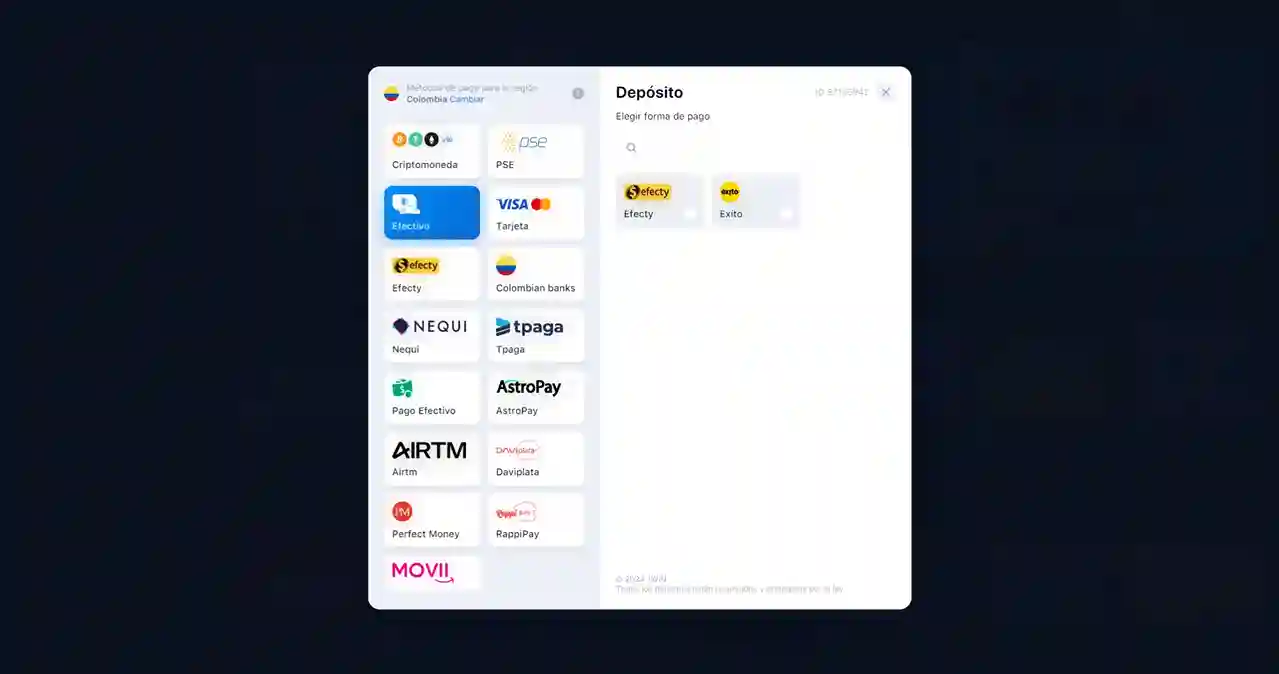
Una de las ventajas de jugar en 1Win Colombia es la amplia gama de métodos de pago disponibles, diseñados para ofrecer comodidad y seguridad a los usuarios. Ya sea que prefieras realizar transacciones desde un dispositivo Android o iOS, la aplicación 1Win facilita el proceso, permitiéndote depositar y retirar fondos de manera rápida y sencilla.
Métodos de Pago Disponibles
1Win Colombia ofrece varias opciones de pago para adaptarse a las necesidades de todos los jugadores. A continuación, se presentan los métodos más populares:
- 1. Tarjetas Bancarias (Visa, Mastercard)
- Las tarjetas de crédito y débito son uno de los métodos de pago más utilizados en 1Win Colombia. Estas transacciones se procesan de manera segura y generalmente se reflejan en la cuenta del usuario de forma inmediata.
- 2. Monederos Electrónicos (Skrill, Neteller)
- Los monederos electrónicos son una opción popular para quienes buscan rapidez y seguridad. Son fáciles de usar y permiten tanto depósitos como retiros de manera eficiente.
- 3. Criptomonedas (Bitcoin, Ethereum)
- Para aquellos que prefieren el anonimato y la seguridad, 1Win acepta pagos en criptomonedas como Bitcoin y Ethereum. Este método es cada vez más popular entre los usuarios que buscan proteger su privacidad.
- 4. Transferencias Bancarias
- Las transferencias bancarias son una opción confiable para quienes prefieren realizar pagos directamente desde su cuenta bancaria. Aunque puede tardar un poco más que otros métodos, es una opción segura y ampliamente disponible.
- 5. Aplicaciones de Pago Móvil
- 1Win Colombia también permite realizar pagos a través de aplicaciones móviles de pago, lo que facilita la gestión de fondos directamente desde tu smartphone.
Uso de la Aplicación 1Win para Pagos
La aplicación 1Win, disponible tanto para Android como para iPhone (iOS), es una herramienta poderosa que hace que la gestión de tus fondos sea más accesible y rápida. Aquí te explicamos cómo puedes usar la 1Win app Android y la 1Win app iPhone para realizar pagos:
- 1Win Android: Si utilizas un dispositivo Android, puedes descargar la 1Win app Android directamente desde el sitio oficial. Una vez instalada, podrás acceder a todas las funciones de la plataforma, incluidos los métodos de pago, de manera rápida y segura.
- 1Win iPhone (iOS): Los usuarios de iPhone también tienen acceso a una versión optimizada de la aplicación 1Win. Disponible para dispositivos iOS, esta app ofrece la misma funcionalidad, permitiéndote realizar depósitos y retiros de manera eficiente y sin complicaciones.
Ventajas de Utilizar la Aplicación 1Win
- Acceso Rápido y Seguro: La aplicación 1Win permite a los usuarios acceder a sus cuentas y realizar transacciones en cualquier momento y desde cualquier lugar, utilizando una conexión segura.
- Notificaciones en Tiempo Real: Recibe notificaciones instantáneas sobre el estado de tus pagos, promociones y actualizaciones de la plataforma.
- Interfaz Intuitiva: Tanto la 1Win app Android como la 1Win app iPhone están diseñadas con una interfaz fácil de usar, lo que hace que la navegación y la gestión de tu cuenta sean sencillas.
Consejos para Maximizar tus Bonos en 1Win
Aprovechar al máximo los bonos y promociones en 1Win puede ser una excelente estrategia para aumentar tus ganancias y disfrutar más de la plataforma. A continuación, te ofrecemos algunos consejos útiles para sacar el máximo provecho de los bonos 1Win, incluyendo cómo utilizar el código promocional GOL5.
1. Usa el Código Promocional Correctamente
Uno de los primeros pasos para maximizar tus bonos en 1Win es utilizar el código promocional GOL5. Este bonus code 1Win: GOL5 te permite acceder a bonos adicionales que pueden no estar disponibles sin el código. Asegúrate de ingresar el 1win código promocional: GOL5 durante el proceso de registro o al hacer tu primer depósito para activar esta oferta.
2. Realiza Depósitos Estratégicos
Para obtener el máximo beneficio del 1win bono, planifica tus depósitos de manera que coincidan con las ofertas de la plataforma. Por ejemplo, si sabes que puedes recibir un bono adicional por un segundo o tercer depósito, asegúrate de tener los fondos necesarios para aprovechar estas promociones.
3. Cumple con los Requisitos de Apuesta
Cada bono 1Win viene con ciertos requisitos de apuesta que debes cumplir antes de poder retirar tus ganancias. Es importante leer y entender estos términos para asegurarte de que puedes cumplirlos. Focalízate en hacer apuestas que cumplan con las condiciones mínimas, como la cuota o el número de veces que el bono debe ser apostado.
4. Participa en Promociones y Eventos Especiales
1Win regularmente ofrece promociones adicionales y eventos especiales que pueden aumentar el valor de tus bonos. Mantente atento a estas oportunidades y participa en ellas para maximizar tus beneficios. Estos eventos a menudo incluyen giros gratis, cashback o bonos adicionales al realizar ciertas actividades.
5. Juega Inteligentemente con tus Bonos
Utiliza tus bonos en juegos o apuestas donde tengas una mayor probabilidad de ganar. Evita realizar apuestas demasiado arriesgadas y enfócate en juegos que ofrezcan un equilibrio entre riesgo y recompensa. Esto te permitirá cumplir con los requisitos de apuesta más rápidamente y maximizar tus ganancias.
6. Revisa las Condiciones Regularmente
Las condiciones de los bonos y los códigos promocionales pueden cambiar, por lo que es esencial revisar las reglas y términos regularmente. Asegúrate de estar al tanto de cualquier cambio para no perder ninguna oportunidad de maximizar tus bonos 1Win.
Resumen
Utilizar el bonus code 1Win: GOL5 y seguir estos consejos te ayudará a aprovechar al máximo las oportunidades de bonos que 1Win ofrece. Planifica estratégicamente, cumple con los requisitos de apuesta, y mantente informado sobre las promociones actuales para sacar el máximo provecho de tus bonos y aumentar tus posibilidades de ganar.
Siguiendo estos consejos, podrás maximizar el valor de tus bonos 1Win y disfrutar de una experiencia de juego más rentable y emocionante.
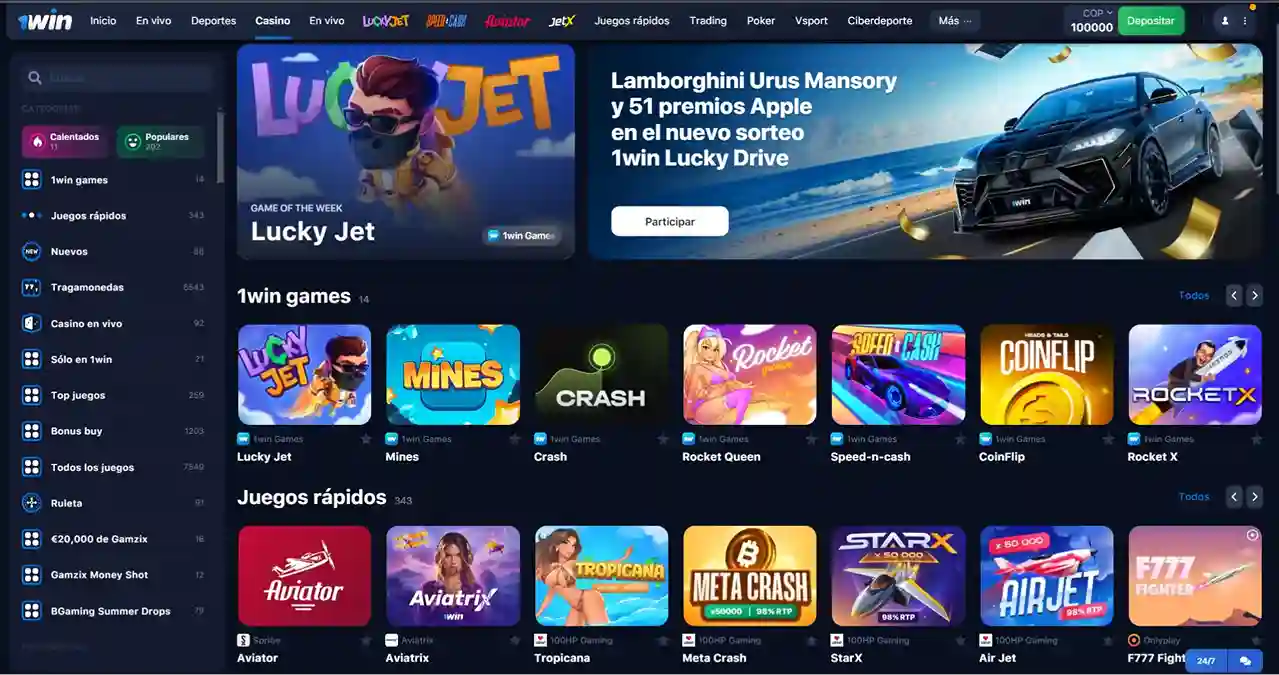
1Win Casino Online: Juegos Disponibles y Promociones
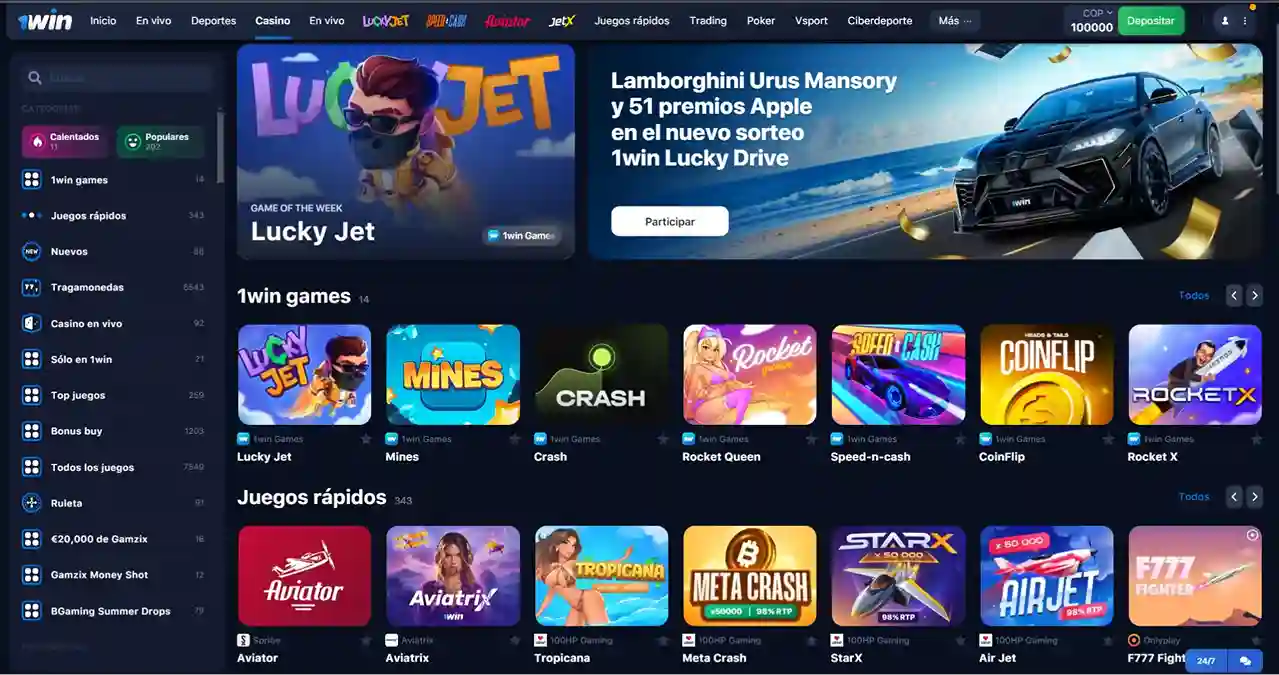
1Win Casino Online ofrece una variada gama de juegos y promociones diseñadas para satisfacer tanto a jugadores nuevos como a experimentados. A continuación, te presentamos una visión general de los principales juegos y las promociones disponibles, con un enfoque especial en Lucky Jet 1Win.
Juegos Disponibles en 1Win Casino
Promociones y Bonos en 1Win Casino
1Win Casino se distingue no solo por su amplia oferta de juegos, sino también por sus atractivas promociones que permiten a los jugadores maximizar su experiencia de juego.
Uso de la 1Win Casino App
Para disfrutar de todos estos juegos y promociones en cualquier momento, 1Win Casino ofrece una aplicación móvil disponible tanto para Android como para iOS.
Para maximizar tus beneficios en 1Win, no olvides utilizar los códigos para 1Win. Por ejemplo, al ingresar el código promocional GOL5 al registrarte o al hacer tu primer depósito, puedes acceder a bonos adicionales y otras promociones especiales que te ayudarán a aumentar tu saldo inicial.
Cómo Contactar con el Soporte de 1Win Colombia
Si necesitas asistencia en 1Win Colombia, puedes contactar con su equipo de soporte de varias maneras, ya sea a través del 1Win website o utilizando la 1Win Colombia app.
- 1. A través del 1Win Website: Visita el sitio oficial de 1Win y navega hasta la sección de soporte. Aquí encontrarás opciones como chat en vivo, correo electrónico, y una sección de preguntas frecuentes que pueden ayudarte a resolver tu problema rápidamente.
- 2. Mediante la 1Win Colombia App: Si prefieres usar tu móvil, la 1Win Colombia app también ofrece acceso directo al soporte al cliente. Dentro de la app, puedes iniciar un chat en vivo o enviar una solicitud de ayuda a través del formulario de contacto.
- 3. Correo Electrónico y Redes Sociales: Además, puedes enviar un correo electrónico directamente a su equipo de soporte o comunicarte a través de sus redes sociales para obtener asistencia adicional.
Estas opciones aseguran que siempre tendrás una manera rápida y fácil de obtener la ayuda que necesitas en 1Win Co.

FAQ para 1Win Colombia
1. ¿Qué es 1Win Colombia?
1Win Colombia es una plataforma en línea que ofrece servicios de casino online y apuestas deportivas. Es conocida por su amplia variedad de juegos, promociones atractivas y accesibilidad desde múltiples dispositivos.
2. ¿Es legal jugar en 1Win Colombia?
1Win opera bajo una licencia internacional válida, lo que permite a los usuarios colombianos utilizar la plataforma sin infringir las leyes locales. Sin embargo, siempre es recomendable verificar las regulaciones locales antes de participar en juegos de azar en línea.
3. ¿Cómo me registro en 1Win Colombia?
Para registrarte en 1Win Colombia, visita el sitio oficial de 1Win y sigue los pasos de registro. Deberás proporcionar información básica como tu nombre, correo electrónico o número de teléfono, y crear una contraseña segura.
4. ¿Cómo puedo obtener el bono de bienvenida en 1Win?
Al registrarte en 1Win y realizar tu primer depósito, recibirás automáticamente un bono de bienvenida de hasta 500%, distribuido en tus primeros cuatro depósitos. No necesitas ingresar un código promocional; el bono se aplica automáticamente.
5. ¿Qué métodos de pago están disponibles en 1Win Colombia?
1Win Colombia ofrece una amplia variedad de métodos de pago, incluidos tarjetas bancarias (Visa, Mastercard), monederos electrónicos (Skrill, Neteller), criptomonedas (Bitcoin, Ethereum), y transferencias bancarias. Además, puedes realizar pagos fácilmente a través de la 1Win app disponible para Android e iOS.
6. ¿Puedo jugar en 1Win desde mi móvil?
Sí, 1Win ofrece una aplicación móvil para Android e iOS. Puedes descargar la 1Win app Android desde el sitio oficial de 1Win, y la 1Win app iPhone está disponible en la App Store. Ambas versiones de la app permiten acceder a todos los juegos y funciones de la plataforma.
7. ¿Qué es Lucky Jet en 1Win?
Lucky Jet es un juego rápido y emocionante disponible en 1Win Casino. Los jugadores apuestan a que un "jet" virtual alcanzará ciertas alturas antes de estrellarse. Es un juego de alto riesgo y alta recompensa que ha ganado popularidad rápidamente.
8. ¿Cómo puedo contactar con el soporte de 1Win Colombia?
Puedes contactar con el equipo de soporte de 1Win Colombia a través de varias opciones:
- Chat en vivo en el sitio oficial de 1Win.
- Soporte en la 1Win Colombia App, disponible para Android e iOS.
- Correo electrónico y redes sociales para obtener asistencia adicional.
9. ¿Cómo puedo retirar mis ganancias en 1Win Colombia?
Para retirar tus ganancias, inicia sesión en tu cuenta de 1Win, dirígete a la sección de retiros, y selecciona el método de pago que prefieras. Asegúrate de haber cumplido con todos los requisitos de apuesta si has utilizado un bono.
10. ¿1Win ofrece promociones especiales o códigos promocionales?
Sí, 1Win ofrece varias promociones especiales. Por ejemplo, puedes usar el código promocional GOL5 para obtener bonos adicionales al registrarte o al hacer tu primer depósito.
 Milán
1 1 0
Milán
1 1 0
 Sassuolo
3 3 0
Sassuolo
3 3 0
 Milán
1 1 0
Milán
1 1 0
 Sassuolo
3 3 0
Sassuolo
3 3 0